Chapter: Paediatrics: Paediatric Surgery
Paediatrics: Congenital abnormalities: tracheo-oesophageal
Congenital abnormalities: tracheo-oesophageal
Tracheo-oesophageal fistula
TOF is usually associated with OA.
However, an isolated TOF will pre-sent with:
•
choking
or coughing during feeding;
•
abdominal
distension;
•
recurrent
LRTI.
Although symptoms are present from
birth the diagnosis is frequently not made until later in childhood. The
investigations of choice are a tube injec-tion of X-ray contrast into the
oesophagus and bronchoscopy. Treatment is surgical division of the TOF through
a neck incision.
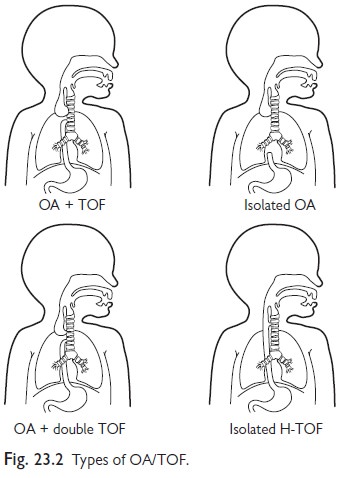
Oesophageal atresia and tracheo-oesophageal fistula
The incidence of OA and TOF (Fig.
23.2) is 1/3500 live births.
•
75%
babies with OA will have a TOF.
•
10%
will have isolated OA, which is usually associated with a long gap or defect.
•
Rare
isolated TOF.
•
Rare
OA with both upper and lower pouch TOFs.
Maternal polyhydramnios is common,
although antenatal diagnosis is rare.
Babies present at birth with:
•
excess
mucus or ‘mucousy’;
•
choking
and cyanosis on feeding;
•
associated
malformations in 50%, usually the VACTERL association.
Diagnosis
Confirmed or excluded by:
•
Passage
of a 10F NGT.
•
CXR: the tube stops in the upper
thorax. Air in the stomach indicates a
fistula between the trachea and the distal oesophagus (TOF).
Acute management
•
The
baby should be kept warm and disturbed as little as possible.
•
The
upper oesophageal pouch should be aspirated regularly by oropharyngeal suction
or a Replogle tube.
•
Standard
IV fluids started.
•
Pre-operative
antibiotics are not required unless there is evidence of aspiration pneumonia.
•
Babies
who require mechanical ventilation must be referred urgently for surgery
because gas will escape down the TOF and produce progressive gastric
distension, which impairs ventilation further, ultimately leading to gastric
perforation.
Surgery
•
Disconnection
of the TOF and anastomosis of upper and lower oesophagus through a right
thoracotomy.
•
Long
gap OA may require a feeding gastrostomy and a cervical oesophagostomy in the
neonatal period followed by oesophageal replacement during infancy. Some
specialist centres now perform the Foker operation, where prolonged internal
‘stretch’ makes the remnant of the upper and lower oesophagus ‘grow’!
•
High-risk
babies may have a staged procedure—the TOF is ligated and then the OA repaired
a few days later.
•
Complications
include anastomotic leak, anastomotic stricture, gastro-oesophageal, and
recurrent fistula.
Follow-up
•
Respiratory
morbidity in the early years after OA/TOF repair is relatively high,
particularly in the winter months. Consider admitting these children during
respiratory infections.
•
Obstruction
of the oesophagus by food boluses is common in toddlers and young children
after OA repair. Usually, it is caused by meat that has not been chewed. Refer
for urgent oesophagoscopy.
Related Topics