Chapter: Medical Surgical Nursing: Management of Patients With Neurologic Trauma
Nursing Process: The Patient With Acute Spinal Cord Injury
NURSING PROCESS: THE PATIENT WITH
ACUTE SPINAL CORD INJURY
Assessment
The breathing pattern is observed, the strength of the
cough is as-sessed, and the lungs are auscultated, because paralysis of
ab-dominal and respiratory muscles diminishes coughing and makes it difficult
to clear bronchial and pharyngeal secretions. Reduced excursion of the chest
also results.
The patient is monitored
closely for any changes in motor or sensory function and for symptoms of
progressive neurologic dam-age. It may be impossible in the early stages of SCI
to determine whether the cord has been severed, because signs and symptoms of
cord edema are indistinguishable from those of cord transection. Edema of the
spinal cord may occur with any severe cord injury and may further compromise
spinal cord function.
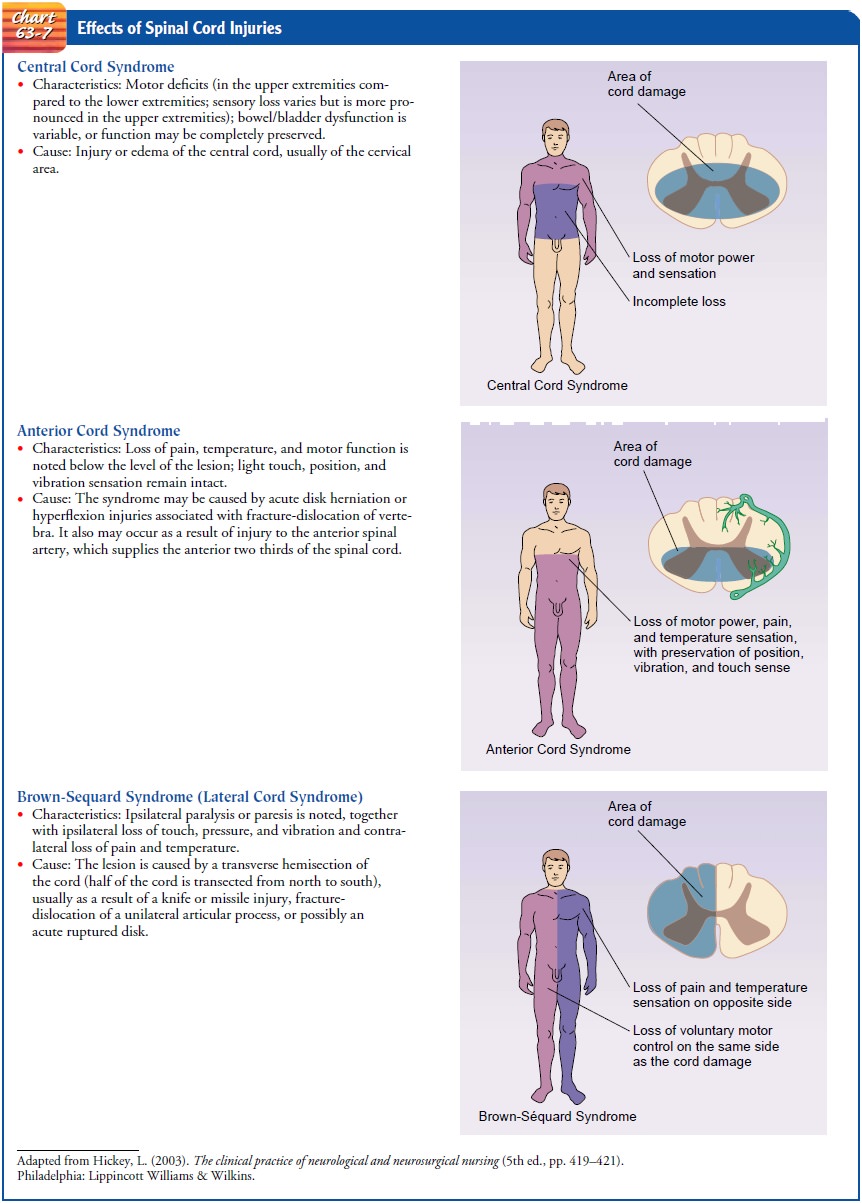
Motor and sensory
functions are assessed through careful neu-rologic examination. These findings
are recorded most often on a flow sheet so that changes in the baseline
neurologic status can be closely monitored accurately. The American Spinal
Injury Associ-ation (ASIA) classification is commonly used to describe level of
function for SCI patients. Chart 63-7 also gives an example of nursing
assessment of spinal cord function.
·
Motor
ability is tested by asking the patient to spread the fingers, squeeze the
examiner’s hand, and move the toes or turn the feet.
·
Sensation is evaluated by
gently pinching the skin or touch-ing it lightly with a small object such as a
tongue blade, starting at shoulder level and working down both sides of the
extremities. The patient should have both eyes closed so that the examination
reveals true findings, not what the pa-tient hopes to feel. The patient is
asked where the sensation is felt.
·
Any decrease in neurologic
function is reported immediately.
The patient is also assessed for spinal shock, a complete
loss of all reflex, motor, sensory, and autonomic activity below the level of
the lesion that causes bladder paralysis and distention. The lower abdomen is
palpated for signs of urinary retention and overdistention of the bladder.
Further assessment is made for gastric dilation and ileus due to an atonic
bowel, a result of auto-nomic disruption.
Temperature is monitored because the patient may have
peri-ods of hyperthermia as a result of alteration in temperature control due
to autonomic disruption.
Diagnosis
NURSING DIAGNOSES
Based on the assessment data, the patient’s major nursing
diag-noses may include the following:
·
Ineffective breathing patterns
related to weakness or paral-ysis of abdominal and intercostal muscles and
inability to clear secretions
·
Ineffective airway clearance
related to weakness of inter-costal muscles
·
Impaired physical mobility
related to motor and sensory impairment
·
Disturbed sensory perception
related to motor and sensory impairment
·
Risk for impaired skin
integrity related to immobility and sensory loss
·
Urinary retention related to
inability to void spontaneously
·
Constipation related to
presence of atonic bowel as a result of autonomic disruption
·
Acute pain and discomfort
related to treatment and pro-longed immobility
COLLABORATIVE PROBLEMS/ POTENTIAL COMPLICATIONS
Based on the assessment data, potential complications
that may develop include:
·
DVT
·
Orthostatic hypotension
·
Autonomic dysreflexia
Planning and Goals
The goals for the patient may include improved breathing
pat-tern and airway clearance, improved mobility, improved sensory and
perceptual awareness, maintenance of skin integrity, relief of urinary
retention, improved bowel function, promotion of com-fort, and absence of
complications.
Nursing Interventions
PROMOTING ADEQUATE BREATHING AND AIRWAY CLEARANCE
Possible impending respiratory failure is detected by
observing the patient, measuring vital capacity, monitoring oxygen satura-tion
through pulse oximetry, and monitoring arterial blood gas values. Early and
vigorous attention to clearing bronchial and pharyngeal secretions can prevent
retention of secretions and at-electasis. Suctioning may be indicated, but
caution must be used during suctioning because this procedure can stimulate the
vagus nerve, producing bradycardia, which can result in cardiac arrest.
If the patient cannot cough effectively because of
decreased in-spiratory volume and inability to generate sufficient expiratory
pressure, chest physical therapy and assisted coughing may be in-dicated.
Specific breathing exercises are supervised by the nurse to increase the
strength and endurance of the inspiratory muscles, particularly the diaphragm.
Assisted coughing promotes clearing of secretions from the upper respiratory
tract and is similar to using abdominal thrusts to clear an airway. It is
important to ensure proper humidification and hydration to pre-vent secretions
from becoming thick and difficult to remove even with coughing. The patient is
assessed for signs of respiratory in-fection (cough, fever, dyspnea). Smoking
is discouraged because it increases bronchial and pulmonary secretions and
impairs ciliary action.
Ascending edema of the spinal cord in the acute phase may
cause respiratory difficulty that requires immediate intervention. Therefore,
the patient’s respiratory status must be monitored frequently.
IMPROVING MOBILITY
Proper body alignment is maintained at all times. The
patient is repositioned frequently and is assisted out of bed as soon as the
spinal column is stabilized. The feet are prone to footdrop; therefore, various
types of splints are used to prevent footdrop. When used, the splints are
removed and reapplied every 2 hours. Trochanter rolls, applied from the crest
of the ilium to the midthigh of both legs, help prevent external rotation of
the hip joints.
Patients with lesions above the midthoracic level have
loss of sympathetic control of peripheral vasoconstrictor activity, lead-ing to
hypotension. These patients may tolerate changes in posi-tion poorly and
require monitoring of blood pressure when positions are changed. Usually the
patient is turned every 2 hours. If not on a rotating bed, the patient should
not be turned unless the spine is stable and the physician has indicated that
it is safe to do so.
Contractures develop rapidly with immobility and muscle
paralysis. A joint that is immobilized too long becomes fixed as a result of
contractures of the tendon and joint capsule. Atrophy of the extremities
results from disuse. Contractures and other com-plications may be prevented by
range-of-motion exercises that help preserve joint motion and stimulate
circulation. Passive range-of-motion exercises should be implemented as soon as
possible after injury. Toes, metatarsals, ankles, knees, and hips should be put
through a full range of motion at least four, and ideally five, times daily.
For most patients with a cervical fracture without
neurologic deficit, reduction in traction followed by rigid immobilization for
about 6 to 8 weeks restores skeletal integrity. These patients are allowed to
move gradually to an erect position. A four-poster neck brace or molded collar
is applied when the patient is mobi-lized after traction is removed (see Fig.
63-8).
PROMOTING ADAPTATION TO SENSORY AND PERCEPTUAL ALTERATIONS
The nurse assists the patient to compensate for sensory
and per-ceptual alterations that occur with SCI. The intact senses above the
level of the injury are stimulated through touch, aromas, flavorful food and
beverages, conversation, and music. Additional strategies include the
following:
·
Providing prism glasses to
enable the patient to see from the supine position
·
Encouraging use of hearing
aids, if indicated, to enable the patient to hear conversations and
environmental sounds
·
Providing emotional support to
the patient
·
Teaching the patient
strategies to compensate for or cope with these deficits
MAINTAINING SKIN INTEGRITY
Because the patient with
SCI is immobilized and has loss of sen-sation below the level of the lesion,
there is an ever-present, life-threatening risk of pressure ulcers. In areas of
local tissue ischemia, where there is continuous pressure and where the
peripheral cir-culation is inadequate as a result of the spinal shock and
recum-bent position, pressure ulcers have developed within 6 hours. Prolonged
immobilization of the patient on a transfer board in-creases the risk of
pressure ulcers. The most common sites are over the ischial tuberosity, the
greater trochanter, and the sacrum. In addition, patients who wear cervical
collars for prolonged pe-riods may develop breakdown from the pressure of the
collar under the chin, on the shoulders, and at the occiput.
The patient’s position
is changed at least every 2 hours. Turn-ing not only assists in the prevention
of pressure ulcers but also pre-vents the pooling of blood and tissue fluid in
the dependent areas.
Careful inspection of
the skin is made each time the patient is turned. The skin over the pressure
points is assessed for redness or breaks; the perineum is checked for soilage
and the catheter is observed for adequate drainage. The patient’s general body
align-ment and comfort are assessed. Special attention should be given to
pressure areas in contact with the transfer board.
The patient’s skin
should be kept clean by washing with a mild soap, rinsed well, and blotted dry.
Pressure-sensitive areas should be kept well lubricated and soft with bland
cream or lotion. The patient is informed about the danger of pressure ulcers to
en-courage understanding of the reason for preventive measures.
MAINTAINING URINARY ELIMINATION
Immediately after SCI, the urinary bladder becomes atonic
and cannot contract by reflex activity. Urinary retention is the imme-diate
result. Because the patient has no sensation of bladder dis-tention,
overstretching of the bladder and detrusor muscle may occur, delaying the
return of bladder function.
Intermittent
catheterization is carried out to avoid over-distention of the bladder and UTI.
If this is not feasible, an in-dwelling catheter is inserted temporarily. At an
early stage, family members are shown how to carry out intermittent
catheterization and are encouraged to participate in this facet of care,
because they will be involved in long-term follow-up and must be able to
recognize complications so that treatment can be instituted.
The patient is taught to
record fluid intake, voiding pattern, amounts of residual urine after
catheterization, characteristics of urine, and any unusual sensations that may
occur.
IMPROVING BOWEL FUNCTION
Immediately after SCI, a paralytic ileus usually develops
due to neurogenic paralysis of the bowel; therefore, a nasogastric tube is
often required to relieve distention and prevent aspiration.
Bowel activity usually returns within the first week. As
soon as bowel sounds are heard on auscultation, the patient is given a
high-calorie, high-protein, high-fiber diet, with the amount of food gradually
increased. The nurse administers prescribed stool softeners to counteract the
effects of immobility and pain med-ications. A bowel program is instituted as
early as possible.
PROVIDING COMFORT MEASURES
After cervical injury, if pins, tongs, or calipers are in
place, the skull is assessed for signs of infection, including drainage. The
back of the head is checked periodically for signs of pressure, with care taken
not to move the neck. The hair around the tongs usu-ally is shaved to
facilitate inspection. Probing under encrusted areas is avoided.
The Patient in Halo Traction
Patients who have been placed in a halo device after
cervical sta-bilization may have a slight headache or discomfort around the skull
pins for several days after the pins are inserted. The patient initially may be
bothered by the rather startling appearance of this apparatus but usually
readily adapts to it because the device pro-vides comfort for the unstable
neck. The patient may complain of being caged in and of noise created by any
object coming in contact with the steel frame, but he or she can be reassured
that adaptation to such annoyances will occur.
The areas around the pin sites are cleansed daily and
observed for redness, drainage, and pain. The pins are observed for loos-ening,
which may contribute to infection. If one of the pins be-comes detached, the
head is stabilized in a neutral position by one person while another notifies
the neurosurgeon. A torque screw-driver should be readily available should the
screws on the frame need tightening.
The skin under the halo
vest is inspected for excessive perspi-ration, redness, and skin blistering,
especially on the bony promi-nences. The vest is opened at the sides to allow
the torso to be washed. The liner of the vest should not become wet, because
dampness causes skin excoriation. Powder is not used inside the vest, because
it may contribute to the development of pressure ul-cers. The liner should be
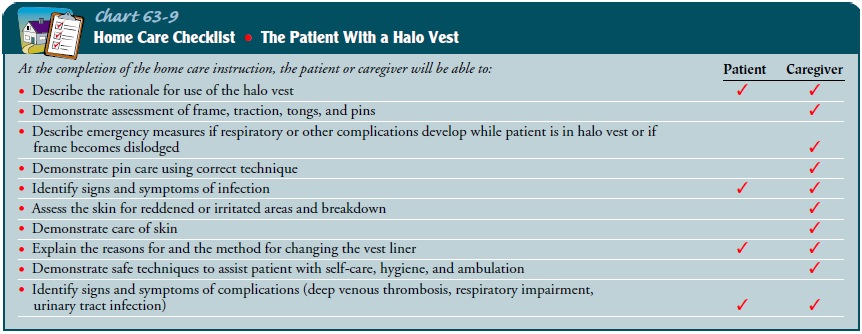
changed periodically to promote hygiene and good skin care. If the patient is
to be discharged with the vest, detailed instructions must be given to the
family and time allowed for them to return demonstrate the necessary skills
(Chart 63-9).
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Thrombophlebitis
Thrombophlebitis is a
relatively common complication in patients after SCI. DVT occurs in a high
percentage of SCI patients; thus, they are at risk for PE. The patient must be
assessed for symptoms of thrombophlebitis and PE: chest pain, shortness of
breath, and changes in arterial blood gas values must be reported promptly to
the physician. The circumferences of the thighs and calves are measured and
recorded daily; further diagnostic studies will be performed if a significant increase
is noted. Patients remain at high risk for thrombophlebitis for several months
after the ini-tial injury. Patients with paraplegia or quadriplegia are at
in-creased risk for the rest of their lives. Immobilization and the associated
venous stasis, as well as varying degrees of autonomic disruption, contribute
to the high risk and susceptibility for DVT (Zafonte et al., 1999).
Anticoagulation is
initiated once head and other systemic in-juries have been ruled out. Low-dose
fractionated or unfraction-ated heparin may be followed by long-term oral
anticoagulation (ie, warfarin) or subcutaneous fractionated heparin injections.
Additional measures such as range-of-motion exercises, thigh-high elastic
compression stockings, and adequate hydration are important preventive
measures. Pneumatic compression devices may also be used to reduce venous
pooling and promote venous return. It is also important to avoid external
pressure on the lower extremities that may result from flexion of the knees
while the patient is in bed.
Orthostatic Hypotension
For the first 2 weeks
after SCI, the blood pressure tends to be un-stable and quite low. There is a
gradual return to preinjury levels, but periodic episodes of severe orthostatic
hypotension frequently interfere with efforts to mobilize the patient.
Interruption in the reflex arcs that normally produce vasoconstriction in the
upright position, coupled with vasodilation and pooling in abdominal and lower
extremity vessels, can result in blood pressure readings of 40 mm Hg systolic
and 0 mm Hg diastolic. Orthostatic hypo-tension is a particularly common
problem for patients with lesions above T7. In some quadriplegic patients, even
slight elevations of the head can result in dramatic changes in blood pressure.
A number of techniques
can be used to reduce the frequency of hypotensive episodes. Close monitoring
of vital signs before and during position changes is essential. Vasopressor
medication can be used to treat the profound vasodilation. Thigh-high elastic
compression stockings should be applied to improve venous re-turn from the
lower extremities. Abdominal binders may also be used to encourage venous
return and provide diaphragmatic sup-port when upright. Activity should be
planned in advance and adequate time given for a slow progression of position
changes from recumbent to sitting and upright. Tilt tables frequently are
helpful in assisting patients to make this transition.
Autonomic Dysreflexia
Autonomic dysreflexia (autonomic hyperreflexia) is an acuteemergency that occurs as a result of exaggerated autonomic re-sponses to stimuli that are harmless in normal people. It occurs only after spinal shock has resolved. This syndrome is characterized by a severe, pounding headache with paroxysmal hypertension, profuse diaphoresis (most often of the forehead), nausea, nasal congestion, and bradycardia. It occurs among patients with cord lesions above T6 (the sympathetic visceral outflow level) after spinal shock has subsided. The sudden rise in blood pressure may cause a rupture of one or more cerebral blood vessels or lead to increased ICP. A number of stimuli may trigger this reflex: distended bladder (the most common cause); distention or con-traction of the visceral organs, especially the bowel (from consti-pation, impaction); or stimulation of the skin (tactile, pain, thermal stimuli, pressure ulcer). Because this is an emergency situation, the objective is to remove the triggering stimulus and to avoid the possibly serious complications.
The following measures are carried out:
·
The patient is placed
immediately in a sitting position to lower blood pressure.
·
Rapid assessment to identify
and alleviate the cause is im-perative.
·
The bladder is emptied
immediately via a urinary catheter. If an indwelling catheter is not patent, it
is irrigated or re-placed with another catheter.
·
The rectum is examined for a
fecal mass. If one is present, a topical anesthetic is inserted 10 to 15
minutes before the mass is removed, because visceral distention or contraction
can cause autonomic dysreflexia.
·
The skin is examined for any
areas of pressure, irritation, or broken skin.
·
Any other stimulus that can be
the triggering event, such as an object on the skin or a draft of cold air,
must be removed.
·
If these measures do not
relieve the hypertension and ex-cruciating headache, a ganglionic blocking
agent (hydralazine hydrochloride [Apresoline]) is prescribed and given slowly
intravenously.
·
The medical record or chart
should be labeled with a clearly visible note about the risk for autonomic
dysreflexia.
·
The patient is instructed
about prevention and manage-ment measures.
·
Any patient with a lesion
above the T6 segment is informed that such an episode is possible and may even
occur many years after the initial injury.
The rehabilitation of the patient with a SCI (ie, the
quadri-plegic or paraplegic patient) is discussed below.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
In most cases, SCI patients need long-term
rehabilitation. The process begins during hospitalization as acute symptoms
begin to subside or come under better control and the overall deficits and
long-term effects of the injury become clear. The goals begin to shift from
merely surviving the injury to learning strategies nec-essary to cope with the
alterations that injury imposes on activi-ties of daily living. The emphasis
shifts from ensuring that the patient is stable and free of complications to
specific assessment and planning designed to meet the patient’s rehabilitation
needs. Patient teaching may initially focus on the injury and its effects on
mobility, dressing, and bowel, bladder, and sexual function. As the patient and
family acknowledge the consequences of the injury, the focus of teaching may
broaden to address issues nec-essary to carry out the tasks of daily living.
Teaching begins in the acute phase and continues throughout rehabilitation and
through-out the patient’s life as changes occur, the patient ages, and problems
arise.
Caring for the SCI patient at home may at first seem a
daunt-ing task to the family. They will require dedicated nursing sup-port to
gradually assume full care of the patient (Craig et al., 1999).
Although maintaining function and preventing
complications will remain important, goals regarding self-care and preparation
for discharge will assist in a smooth transition to rehabilitation and
eventually to the community.
Continuing Care
The ultimate goal of the
rehabilitation process is independence. The nurse becomes a support to both the
patient and the family,assisting them to assume responsibility for increasing
aspects of patient care and management. Care for the SCI patient involves
members of all the health care disciplines; these may include nurs-ing,
medicine, rehabilitation, respiratory therapy, physical and occupational
therapy, case management, social services, and so forth. The nurse often serves
as coordinator of the management team and as a liaison with rehabilitation
centers and home care agencies. The patient and family often require assistance
in deal-ing with the psychological impact of the injury and its conse-quences;
referral to a psychiatric clinical nurse specialist or other mental health care
professional often is helpful.
The nurse should reassure female SCI patients that
pregnancy is not contraindicated, but pregnant women with acute or chronic SCI
pose unique management challenges. The normal physiologic changes of pregnancy
may predispose women with SCI to many potentially life-threatening
complications, includ-ing autonomic dysreflexia, pyelonephritis, respiratory
insuffi-ciency, thrombophlebitis, PE, and unattended delivery (Atterbury &
Groome, 1998).
As more patients survive
acute SCI, they will face the changes associated with aging with a disability.
Thus, teaching in the home and community focuses on health promotion and
ad-dresses the need to minimize risk factors (eg, smoking, alcohol and drug
abuse, obesity). Home care nurses and others who have contact with patients
with SCI are in a position to teach patients about healthy lifestyles, remind
them of the need for health screenings, and make referrals as appropriate.
Assisting patients to identify accessible health care providers and imaging
centers may increase the likelihood that they will participate in health
screening (eg, gynecologic examinations, mammograms, etc.).
Evaluation
EXPECTED PATIENT OUTCOMES
Expected patient outcomes may include:
1) Demonstrates
improvement in gas exchange and clearance of secretions, as evidenced by normal
breath sounds on auscultation
a) Breathes
easily without shortness of breath
b) Performs
hourly deep-breathing exercises, coughs effec-tively, and clears pulmonary
secretions
c) Is
free of respiratory infection (ie, has normal tempera-ture, respiratory rate,
and pulse, normal breath sounds, absence of purulent sputum)
2) Moves
within limits of the dysfunction and demonstrates completion of exercises
within functional limitations
3) Demonstrates
adaptation to sensory and perceptual alter-ations
a) Uses
assistive devices (eg, prism glasses, hearing aids, computers) as indicated
b) Describes
sensory and perceptual alterations as a conse-quence of injury
4) Demonstrates
optimal skin integrity
a) Exhibits
normal skin turgor; skin is free of reddened areas or breaks
b) Participates
in skin care and monitoring procedures within functional limitations
5) Regains
urinary bladder function
a) Exhibits
no signs of UTI (ie, has normal temperature; voids clear, dilute urine)
b) Has
adequate fluid intake
c) Participates
in bladder training program within func-tional limitations
6) Regains
bowel function
a) Reports
regular pattern of bowel movement
b) Consumes
adequate dietary fiber and oral fluids
c) Participates
in bowel training program within func-tional limitations
7) Reports
absence of pain and discomfort
8) Is
free of complications
a) Demonstrates
no signs of thrombophlebitis, DVT, or PE
b) Exhibits
no manifestations of pulmonary embolism (eg, no chest pain or shortness of
breath; arterial blood gas values are normal)
c) Maintains
blood pressure within normal limits
d) Has
no lightheadedness with position changes
e) Exhibits
no manifestations of autonomic dysreflexia (ie, no headache, diaphoresis, nasal
congestion, brady-cardia, or diaphoresis)
Management of the Quadriplegic or Paraplegic Patient
Quadriplegia refers to the loss of movement and sensation
in all four extremities and the trunk, associated with injury to the cer-vical
spinal cord. Paraplegia refers to loss of motion and sensation in the lower
extremities and all or part of the trunk as a result of damage to the thoracic
or lumbar spinal cord or to the sacral root. Both conditions most frequently
follow trauma such as falls, in-juries, and gunshot wounds, but they may also
be the result of spinal cord lesions (intervertebral disk, tumor, vascular
lesions), multiple sclerosis, infections and abscesses of the spinal cord, and
congenital disorders.
The patient faces a
lifetime of great disability, requiring on-going follow-up and care and the
expertise of a number of health professionals, including physicians
(specifically a physiatrist), re-habilitation nurses, occupational therapist,
physical therapist, psychologist, social worker, rehabilitation engineer, and
voca-tional counselor at different times as the need arises.
As the years go by, these patients also have the same
medical problems as others in the aging population. In addition, they face the
threat of complications associated with their disability. Usu-ally the patient
is encouraged to attend a spinal clinic when com-plications and other issues
arise. Lifetime care includes assessment of the urinary tract at prescribed
intervals, because there is the likelihood of continuing alteration in detrusor
and sphincter function and the patient is prone to UTI.
Long-term problems and
complications of SCI include disuse syndrome, autonomic dysreflexia (discussed
earlier), bladder and kidney infections, spasticity, and depression. Pressure
ulcers with potential complications of sepsis, osteomyelitis, and fistulas
occur in about 10% of patients. Flexor muscle spasms may be particu-larly
disabling and occur in up to 25% of patients (Sullivan, 1999). Heterotopic
ossification (overgrowth of bone) in the hips, knees, shoulders, and elbows
occurs in up to 30% of SCI patients. This complication is painful and can
produce a loss of range of motion (Mitcho & Yanko, 1999; Subbarao &
Garrison, 1999). Management includes observing for and addressing any
alter-ation in physiologic status and psychological outlook, and the prevention
and treatment of long-term complications. The nurs-ing role involves emphasizing
the need for vigilance in self-assessment and care.
Related Topics