Chapter: Basic & Clinical Pharmacology : Agents Used in Dyslipidemia
NIACIN (Nicotinic Acid)
NIACIN (NICOTINIC ACID)
Niacin (but not
niacinamide) decreases VLDL and LDL levels, and Lp(a) in most patients. It
often increases HDL levels signifi-cantly.
Chemistry & Pharmacokinetics
Niacin (vitamin B3) is converted in the
body to the amide, which is incorporated into niacinamide adenine dinucleotide
(NAD). It is excreted in the urine unmodified and as several metabolites.
Mechanism of Action
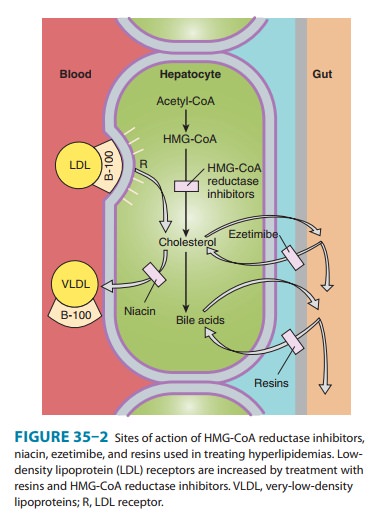
Niacin inhibits VLDL
secretion, in turn decreasing production of LDL (Figure 35–2). Increased
clearance of VLDL via the LPL pathway contributes to reduction of
triglycerides. Niacin has no effect on bile acid production. Excretion of
neutral sterols in the stool is increased acutely as cholesterol is mobilized
from tissue pools and a new steady state is reached. The catabolic rate for HDL
is decreased. Fibrinogen levels are reduced, and levels of tissue plasminogen
activator appear to increase. Niacin inhibits the intracellular lipase of
adipose tissue via receptor-mediated signaling, possibly reducing VLDL
production by decreasing the flux of free fatty acids to the liver. Sustained
inhibition of lipolysis has not been established, however.
Therapeutic Uses & Dosage
In combination with a
resin or reductase inhibitor, niacin normal-izes LDL in most patients with
heterozygous familial hypercholes-terolemia and other forms of
hypercholesterolemia. These combinations are also indicated in some cases of
nephrosis. In severe mixed lipemia that is incompletely responsive to diet,
niacin often produces marked reduction of triglycerides, an effect enhanced by
marine omega-3 fatty acids. It is useful in patients with combined
hyperlipidemia and in those with dysbetalipopro-teinemia. It is clearly the
most effective agent for increasing HDL and the only agent that may reduce
Lp(a).
For treatment of
heterozygous familial hypercholesterolemia, most patients require 2–6 g of
niacin daily; more than this should not be given. For other types of
hypercholesterolemia and for hypertriglyceridemia, 1.5–3.5 g daily is often
sufficient. Crystalline niacin should be given in divided doses with meals,
starting with 100 mg two or three times daily and increasing gradually.
Toxicity
Most
persons experience a harmless cutaneous vasodilation and sensation of warmth
after each dose when niacin is started or the dose increased. Taking 81–325 mg
of aspirin one half hour before-hand blunts this prostaglandin-mediated effect.
Ibuprofen, once daily, also mitigates the flush. Tachyphylaxis to flushing
usually occurs within a few days at doses above 1.5–3 g daily. Patients should
be warned to expect the flush and understand that it is a harmless side effect.
Pruritus, rashes, dry skin or mucous mem-branes, and acanthosis nigricans have
been reported. The latter contraindicates use of niacin because of its
association with insulin resistance. Some patients experience nausea and
abdominal dis-comfort. Many can continue the drug at reduced dosage, with
inhibitors of gastric acid secretion or with antacids not containing aluminum.
Niacin should be avoided in most patients with severe peptic disease.
Reversible
elevations in aminotransferases up to twice normal may occur, usually not
associated with liver toxicity. However, liver function should be monitored at
baseline and at appropriate intervals. Rarely, true hepatotoxicity may occur,
and in these cases the drug should be discontinued. The association of severe
hepatic dysfunction, including acute necrosis, with the use of over-the-counter
sustained-release preparations of niacin has been reported. This effect has not
been noted to date with an extended-release preparation, Niaspan, given at
bedtime in doses of 2 g or less. Carbohydrate tolerance may be moderately
impaired, especially in obese patients, but this is usually reversible except
in some patients with latent diabetes. Niacin may be given to diabetics who are
receiving insulin and to some receiving oral agents. Niacin may increase
insulin resistance in some patients. This can often be addressed by increasing
the dose of insulin or the oral agents. Hyperuricemia occurs in some patients
and occasionally precipi-tates gout. Allopurinol can be given with niacin if
needed. Red cell macrocytosis is frequently observed with higher doses of
niacin and is not an indication for discontinuing treatment. Significant
platelet deficiency can occur rarely and is reversible on cessation of
treatment. Rarely, niacin is associated with arrhythmias, mostly atrial, and
with macular edema. Patients should be instructed to report blurring of
distance vision. Niacin may potentiate the action of antihypertensive agents,
requiring adjustment of their dosages. Birth defects have been reported in
animals given very high doses.
Related Topics