Chapter: Medical Physiology: Pulmonary Ventilation
Mechanics of Pulmonary Ventilation
Mechanics of Pulmonary Ventilation
Muscles That Cause Lung Expansion and Contraction
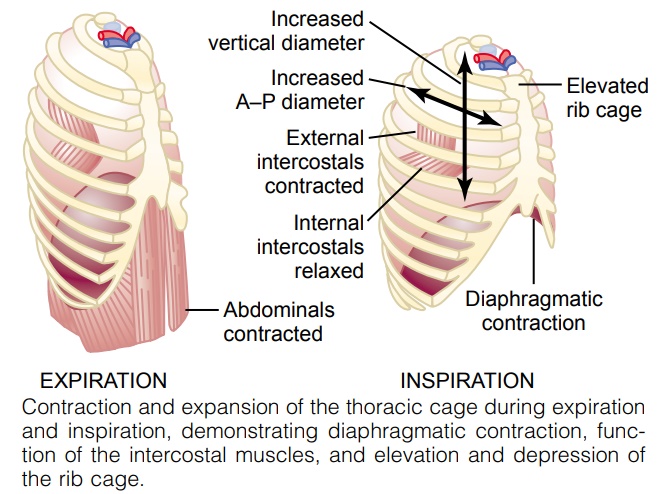
The lungs can be expanded and contracted in two ways: (1) by downward and upward movement of the diaphragm to lengthen or shorten the chest cavity, and (2) by elevation and depression of the ribs to increase and decrease the anteroposterior diameter of the chest cavity. Figure 37–1 shows these two methods.
Normal quiet breathing is accomplished almost entirely by the first method, that is, by movement of the diaphragm. During inspiration, contraction of the diaphragm pulls the lower surfaces of the lungs downward. Then, during expi-ration, the diaphragm simply relaxes, and the elastic recoil of the lungs, chest wall, and abdominal structures compresses the lungs and expels the air. During heavy breathing, however, the elastic forces are not powerful enough to cause the necessary rapid expiration, so that extra force is achieved mainly by con-traction of the abdominal muscles, which pushes the abdominal contents upward against the bottom of the diaphragm, thereby compressing the lungs.
The second method for expanding the lungs is to raise the rib cage. This expands the lungs because, in the natural resting position, the ribs slant down-ward, as shown on the left side of Figure 37–1, thus allowing the sternum to fall backward toward the vertebral column. But when the rib cage is elevated, the ribs project almost directly forward, so that the sternum also moves forward, away from the spine, making the anteroposterior thickness of the chest about 20 per cent greater during maximum inspiration than during expiration. There-fore, all the muscles that elevate the chest cage are classified as muscles of inspi-ration, and those muscles that depress the chest cage are classified as muscles of expiration. The most important muscles that raise the rib cage are the exter-nal intercostals, but others that help are the (1) sternocleidomastoid muscles,which lift upward on the sternum; (2) anterior serrati, which lift many of the ribs; and (3) scaleni, which lift the first two ribs.
The muscles that pull the rib cage downward during expiration are mainly the (1) abdominal recti, which have the powerful effect of pulling downward on the lower ribs at the same time that they and other abdominal muscles also com-press the abdominal contents upward against the diaphragm, and (2) internalintercostals.
Figure 37–1 also shows the mechanism by which the external and internal intercostals act to cause inspira-tion and expiration. To the left, the ribs during expiration are angled downward, and the external intercostals are elongated forward and downward. As they contract, they pull the upper ribs forward in rela-tion to the lower ribs, and this causes leverage on the ribs to raise them upward, thereby causing inspiration. The internal intercostals function exactly in the oppo-site manner, functioning as expiratory muscles because they angle between the ribs in the opposite direction and cause opposite leverage.
Movement of Air In and Out of the Lungs and the Pressures That Cause the Movement
The lung is an elastic structure that collapses like a balloon and expels all its air through the trachea when-ever there is no force to keep it inflated. Also, there are no attachments between the lung and the walls of the chest cage, except where it is suspended at its hilum from the mediastinum. Instead, the lung “floats” in the thoracic cavity, surrounded by a thin layer of pleuralfluid that lubricates movement of the lungs within thecavity. Further, continual suction of excess fluid into lymphatic channels maintains a slight suction between the visceral surface of the lung pleura and the parietal pleural surface of the thoracic cavity. Therefore, the lungs are held to the thoracic wall as if glued there, except that they are well lubricated and can slide freely as the chest expands and contracts.
Pleural Pressure and Its Changes During Respiration
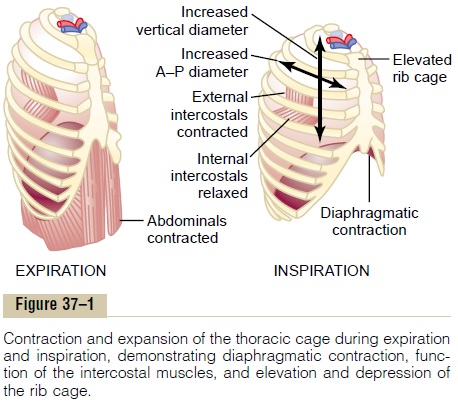
Pleural pressure is the pressure of the fluid in the thinspace between the lung pleura and the chest wall pleura. As noted earlier, this is normally a slight suction, which means a slightly negative pressure. The normal pleural pressure at the beginning of inspiration is about –5 centimeters of water, which is the amount of suction required to hold the lungs open to their resting level. Then, during normal inspiration, expan-sion of the chest cage pulls outward on the lungs with greater force and creates more negative pressure, to an average of about –7.5 centimeters of water.
These relationships between pleural pressure and changing lung volume are demonstrated in Figure 37–2, showing in the lower panel the increasing nega-tivity of the pleural pressure from –5 to –7.5 during inspiration and in the upper panel an increase in lung volume of 0.5 liter. Then, during expiration, the events are essentially reversed.
Alveolar Pressure
Alveolar pressure is the pressure of the air inside thelung alveoli. When the glottis is open and no air is flowing into or out of the lungs, the pressures in all parts of the respiratory tree, all the way to the alveoli, are equal to atmospheric pressure, which is considered to be zero reference pressure in the airways—that is, 0 centimeters water pressure. To cause inward flow of air into the alveoli during inspiration, the pressure in the alveoli must fall to a value slightly below atmos-pheric pressure (below 0). The second curve (labeled “alveolar pressure”) of Figure 37–2 demonstrates that during normal inspiration, alveolar pressure decreases to about –1 centimeter of water. This slight negative pressure is enough to pull 0.5 liter of air into the lungs in the 2 seconds required for normal quiet inspiration.
During expiration, opposite pressures occur: The alveolar pressure rises to about +1 centimeter of water, and this forces the 0.5 liter of inspired air out of the lungs during the 2 to 3 seconds of expiration.
Transpulmonary Pressure. Finally, note in Figure 37–2 thedifference between the alveolar pressure and the pleural pressure. This is called the transpulmonarypressure. It is the pressure difference between that inthe alveoli and that on the outer surfaces of the lungs, and it is a measure of the elastic forces in the lungs that tend to collapse the lungs at each instant of res-piration, called the recoil pressure.
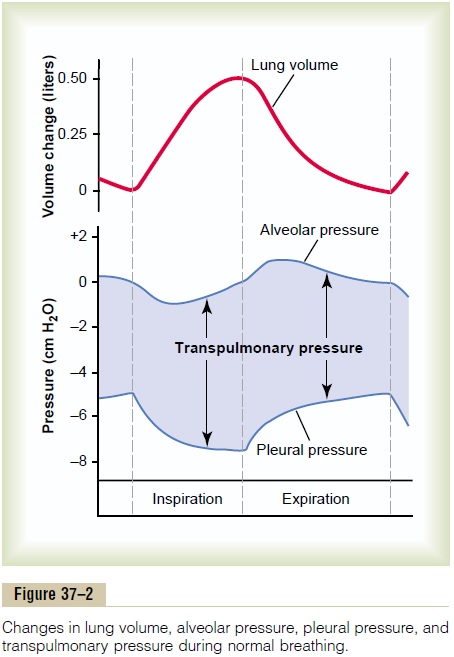
Compliance of the Lungs The extent to which the lungs will expand for each unit increase in transpulmonary pressure (if enough time is allowed to reach equilibrium) is called the lung com-pliance. The total compliance of both lungs together inthe normal adult human being averages about 200 mil-liliters of air per centimeter of water transpulmonary pressure. That is, every time the transpulmonary pres-sure increases 1 centimeter of water, the lung volume, after 10 to 20 seconds, will expand 200 milliliters.
Compliance Diagram of the Lungs. Figure 37–3 is a diagramrelating lung volume changes to changes in transpul-monary pressure. Note that the relation is different for inspiration and expiration. Each curve is recorded by changing the transpulmonary pressure in small steps and allowing the lung volume to come to a steady level
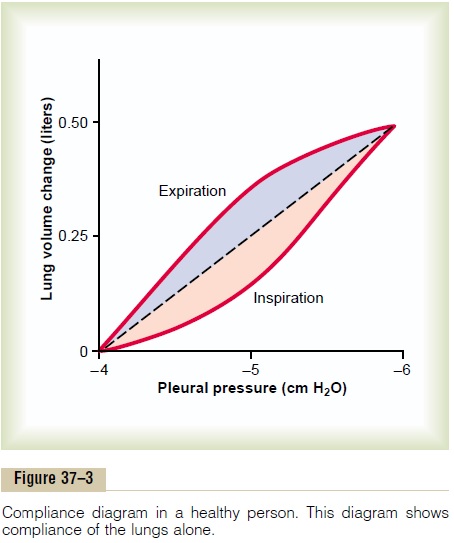
between successive steps. The two curves are called, respectively, the inspiratory compliance curve and the expiratory compliance curve, and the entire diagram iscalled the compliance diagram of the lungs.
The characteristics of the compliance diagram are determined by the elastic forces of the lungs. These can be divided into two parts: (1) elastic forces of the lungtissue itself and (2) elastic forces caused by surface tension of the fluid that lines the inside walls of the alveoli and other lung air spaces.
The elastic forces of the lung tissue are determined mainly by elastin and collagen fibers interwoven among the lung parenchyma. In deflated lungs, these fibers are in an elastically contracted and kinked state; then, when the lungs expand, the fibers become stretched and unkinked, thereby elongating and exert-ing even more elastic force.
The elastic forces caused by surface tension are much more complex. The significance of surface tension is shown in Figure 37–4, which compares the compliance diagram of the lungs when filled with saline solution and when filled with air.When the lungs are filled with air, there is an interface between the alveolar fluid and the air in the alveoli. In the case of the saline solution–filled lungs, there is no air-fluid interface; therefore, the surface tension effect is not present—only tissue elastic forces are operative in the saline solution–filled lung.
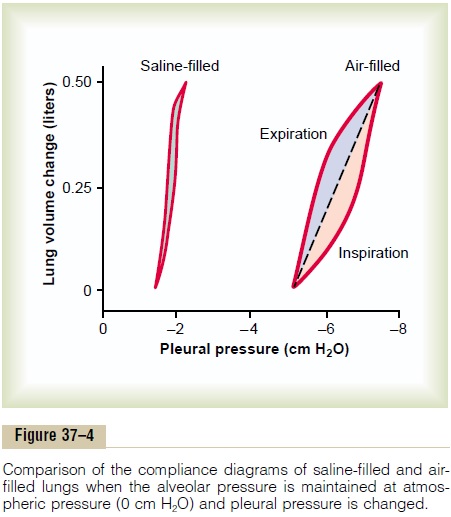
Note that transpleural pressures required to expand air-filled lungs are about three times as great as those required to expand saline solution–filled lungs. Thus, one can conclude that the tissue elastic forces tendingto cause collapse of the air-filled lung represent only about one third of the total lung elasticity, whereas the fluid-air surface tension forces in the alveoli represent about two thirds.
The fluid-air surface tension elastic forces of the lungs also increase tremendously when the substance called surfactant is not present in the alveolar fluid. Let us now discuss surfactant and its relation to the surface tension forces.
Surfactant, Surface Tension, and Collapse of the Alveoli Principle of Surface Tension. When water forms a surfacewith air, the water molecules on the surface of the water have an especially strong attraction for one another. As a result, the water surface is always attempting to contract. This is what holds raindrops together: that is, there is a tight contractile membrane of water molecules around the entire surface of the raindrop. Now let us reverse these principles and see what happens on the inner surfaces of the alveoli. Here, the water surface is also attempting to contract. This results in an attempt to force the air out of the alveoli through the bronchi and, in doing so, causes the alveoli to try to collapse. The net effect is to cause an elastic contractile force of the entire lungs, which is called thesurface tension elastic force.
Surfactant and Its Effect on Surface Tension. Surfactant is asurface active agent in water, which means that itgreatly reduces the surface tension of water. It is secreted by special surfactant-secreting epithelial cells called type II alveolar epithelial cells, which constitute about 10 per cent of the surface area of the alveoli. These cells are granular, containing lipid inclusions that are secreted in the surfactant into the alveoli.
Surfactant is a complex mixture of several phospholipids, proteins, and ions. The most important components are the phospholipiddipalmitoylphos-phatidylcholine, surfactant apoproteins, and calcium ions. The dipalmitoylphosphatidylcholine, along withseveral less important phospholipids, is responsible for reducing the surface tension. It does this by not dissolving uniformly in the fluid lining the alveolar surface. Instead, part of the molecule dissolves, while the remainder spreads over the surface of the water in the alveoli. This surface has from one twelfth to one half the surface tension of a pure water surface.
In quantitative terms, the surface tension of differ-ent water fluids is approximately the following: pure water, 72 dynes/cm; normal fluids lining the alveoli but without surfactant, 50 dynes/cm; normal fluids lining the alveoli and with normal amounts of surfactant included, between 5 and 30 dynes/cm.
Pressure in Occluded Alveoli Caused by Surface Tension. If theair passages leading from the alveoli of the lungs are blocked, the surface tension in the alveoli tends to col-lapse the alveoli. This creates positive pressure in the alveoli, attempting to push the air out. The amount of pressure generated in this way in an alveolus can be cal-culated from the following formula:
Pressure= 2 x Surface tension/ Radius of alveolus
For the average-sized alveolus with a radius of about 100 micrometers and lined with normal surfactant, this calculates to be about 4 centimeters of water pressure (3 mm Hg). If the alveoli were lined with pure water without any surfactant, the pressure would calculate to be about 18 centimeters of water pressure, 4.5 times as great. Thus, one sees how important surfactant is in reducing alveolar surface tension and therefore also reducing the effort required by the respiratory muscles to expand the lungs.
Effect of Alveolar Radius on the Pressure Caused by Surface Tension. Note from the preceding formula that the pres-sure generated as a result of surface tension in the alveoli is inversely affected by the radius of the alveo-lus, which means that the smaller the alveolus, the greater the alveolar pressure caused by the surface tension. Thus, when the alveoli have half the normal radius (50 instead of 100 micrometers), the pressures noted earlier are doubled. This is especially significant in small premature babies, many of whom have alveoli with radii less than one quarter that of an adult person. Further, surfactant does not normally begin to be secreted into the alveoli until between the sixth and seventh months of gestation, and in some cases, even later than that. Therefore, many premature babies have little or no surfactant in the alveoli when they are born, and their lungs have an extreme tendency to collapse, sometimes as great as six to eight times that in a normal adult person. This causes the condition called respira-tory distress syndrome of the newborn. It is fatal ifnot treated with strong measures, especially properly applied continuous positive pressure breathing.
Effect of the Thoracic Cage on Lung Expansibility
Thus far, we have discussed the expansibility of the lungs alone, without considering the thoracic cage. The thoracic cage has its own elastic and viscous charac-teristics, similar to those of the lungs; even if the lungs were not present in the thorax, muscular effort would still be required to expand the thoracic cage.
Compliance of the Thorax and the Lungs Together
The compliance of the entire pulmonary system (the lungs and thoracic cage together) is measured while expanding the lungs of a totally relaxed or paralyzed person. To do this, air is forced into the lungs a little at a time while recording lung pressures and volumes. To inflate this total pulmonary system, almost twice as much pressure is needed as to inflate the same lungs after removal from the chest cage. Therefore, the com-pliance of the combined lung-thorax system is almost exactly one half that of the lungs alone—110 milliliters of volume per centimeter of water pressure for the combined system, compared with 200 ml/cm for the lungs alone. Furthermore, when the lungs are expanded to high volumes or compressed to low volumes, the limitations of the chest become extreme;when near these limits, the compliance of the com-bined lung-thorax system can be less than one fifth that of the lungs alone.
“Work” of Breathing
We have already pointed out that during normal quiet breathing, all respiratory muscle contraction occurs during inspiration; expiration is almost entirely a passive process caused by elastic recoil of the lungs and chest cage. Thus, under resting conditions, the respira-tory muscles normally perform “work” to cause inspi-ration but not to cause expiration.
The work of inspiration can be divided into three fractions: (1) that required to expand the lungs against the lung and chest elastic forces, called compliance work or elastic work; (2) that required to overcome the vis-cosity of the lung and chest wall structures, called tissueresistance work; and (3) that required to overcomeairway resistance to movement of air into the lungs, called airway resistance work.
Energy Required for Respiration. During normal quiet respi-ration, only 3 to 5 per cent of the total energy expended by the body is required for pulmonary ventilation. But during heavy exercise, the amount of energy required can increase as much as 50-fold, especially if the person has any degree of increased airway resistance or de-creased pulmonary compliance. Therefore, one of the major limitations on the intensity of exercise that can be performed is the person’s ability to provide enough muscle energy for the respiratory process alone.
Related Topics