Chapter: Medical Physiology: Pulmonary Ventilation
Functions of the Respiratory Passageways
Functions of the Respiratory Passageways
Trachea, Bronchi, and Bronchioles
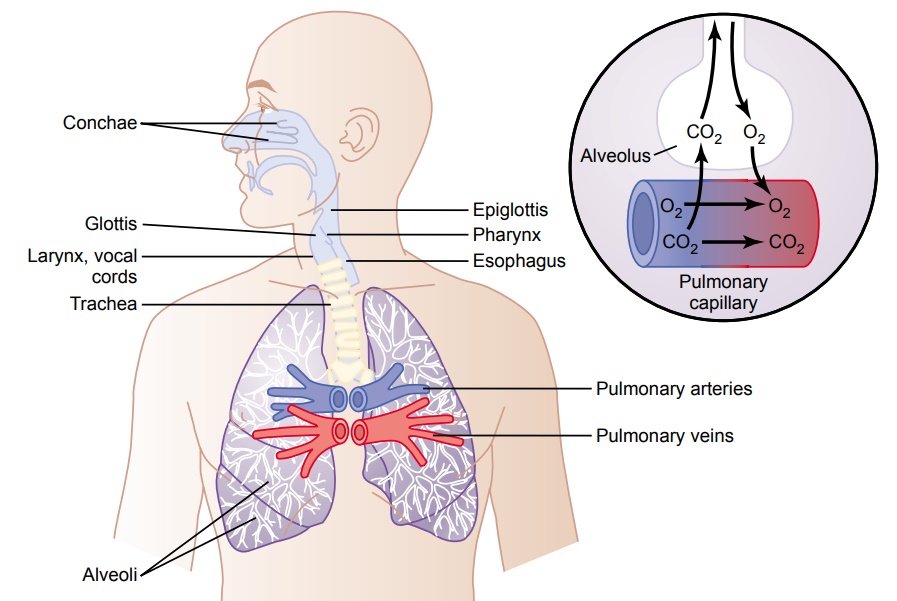
Figure 37–8 shows the respiratory system, demonstrat-ing especially the respiratory passageways. The air is dis-tributed to the lungs by way of the trachea, bronchi, and bronchioles.
One of the most important problems in all the respi-ratory passageways is to keep them open and allow easy passage of air to and from the alveoli. To keep the trachea from collapsing, multiple cartilage rings extend about five sixths of the way around the trachea. In the walls of the bronchi, less extensive curved cartilage plates also maintain a reasonable amount of rigidity yet allow sufficient motion for the lungs to expand and
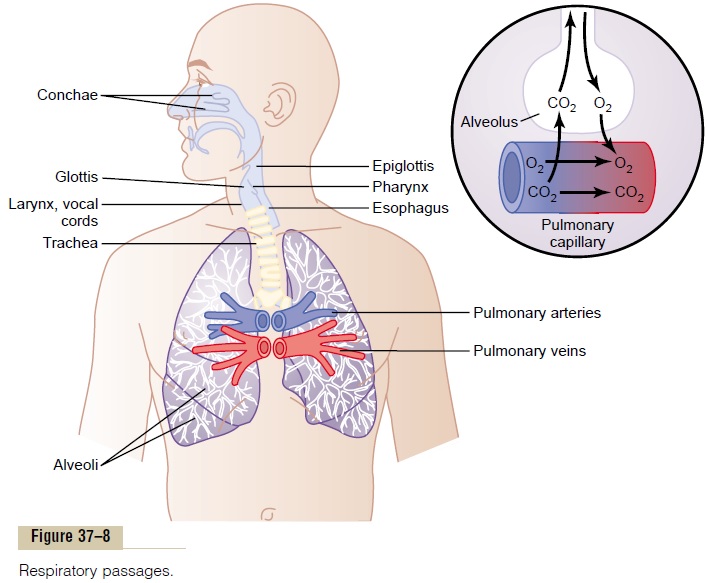
contract. These plates become progressively less exten-sive in the later generations of bronchi and are gone in the bronchioles, which usually have diameters less than 1.5 millimeters. The bronchioles are not prevented from collapsing by the rigidity of their walls. Instead, they are kept expanded mainly by the same transpulmonary pressures that expand the alveoli. That is, as the alveoli enlarge, the bronchioles also enlarge, but not as much.
Muscular Wall of the Bronchi and Bronchioles and Its Control. Inall areas of the trachea and bronchi not occupied by car-tilage plates, the walls are composed mainly of smooth muscle. Also, the walls of the bronchioles are almost entirely smooth muscle, with the exception of the most terminal bronchiole, called the respiratory bronchiole, which is mainly pulmonary epithelium and underlying fibrous tissue plus a few smooth muscle fibers. Many obstructive diseases of the lung result from narrowing of the smaller bronchi and larger bronchioles, often because of excessive contraction of the smooth muscle itself.
Resistance to Airflow in the Bronchial Tree. Undernormalrespiratory conditions, airflows through the respiratorypassageways so easily that less than 1 centimeter of water pressure gradient from the alveoli to the atmos-phere is sufficient to cause enough airflow for quiet breathing. The greatest amount of resistance to airflow occurs not in the minute air passages of the terminal bronchioles but in some of the larger bronchioles and bronchi near the trachea. The reason for this high resist-ance is that there are relatively few of these larger bronchi in comparison with the approximately 65,000 parallel terminal bronchioles, through each of which only a minute amount of air must pass.
Yet in disease conditions, the smaller bronchioles often play a far greater role in determining airflow resistance because of their small size and because they are easily occluded by (1) muscle contraction in their walls, (2) edema occurring in the walls, or (3) mucus col-lecting in the lumens of the bronchioles.
Nervous and Local Control of the Bronchiolar Musculature— “Sympathetic” Dilation of the Bronchioles. Direct control ofthe bronchioles by sympathetic nerve fibers is relatively weak because few of these fibers penetrate to the central portions of the lung. However, the bronchial tree is very much exposed to norepinephrine and epineph-rine released into the blood by sympathetic stimulationof the adrenal gland medullae. Both these hormones— especially epinephrine, because of its greater stimula-tion of beta-adrenergic receptors—cause dilation of the bronchial tree.
Parasympathetic Constriction of the Bronchioles. A fewparasympathetic nerve fibers derived from the vagus nerves penetrate the lung parenchyma. These nerves secrete acetylcholine and, when activated, cause mild to moderate constriction of the bronchioles. When a disease process such as asthma has already caused some bronchiolar constriction, superimposed parasympa-thetic nervous stimulation often worsens the condition. When this occurs, administration of drugs that block the effects of acetylcholine, such asatropine, can sometimes relax the respiratory passages enough to relieve the obstruction.
Sometimes the parasympathetic nerves are also acti-vated by reflexes that originate in the lungs. Most of these begin with irritation of the epithelial membrane of the respiratory passageways themselves, initiated by noxious gases, dust, cigarette smoke, or bronchial infec-tion. Also, a bronchiolar constrictor reflex often occurs when microemboli occlude small pulmonary arteries.
Local Secretory Factors Often Cause Bronchiolar Constriction.Several substances formed in the lungs themselves are often quite active in causing bronchiolar constriction. Two of the most important of these are histamine and slow reactive substance of anaphylaxis. Both of these arereleased in the lung tissues by mast cells during allergic reactions, especially those caused by pollen in the air. Therefore, they play key roles in causing the airway obstruction that occurs in allergic asthma; this is espe-cially true of the slow reactive substance of anaphylaxis.
The same irritants that cause parasympathetic con-strictor reflexes of the airways—smoke, dust, sulfur dioxide, and some of the acidic elements in smog—often act directly on the lung tissues to initiate local, non-nervous reactions that cause obstructive constriction of the airways.
Mucus Lining the Respiratory Passageways, and Action of Cilia to Clear the Passageways
All the respiratory passages, from the nose to the ter-minal bronchioles, are kept moist by a layer of mucus that coats the entire surface. The mucus is secreted partly by individual mucous goblet cells in the epithe-lial lining of the passages and partly by small submu-cosal glands. In addition to keeping the surfaces moist, the mucus traps small particles out of the inspired air and keeps most of these from ever reaching the alveoli. The mucus itself is removed from the passages in the following manner.
The entire surface of the respiratory passages, both in the nose and in the lower passages down as far as the terminal bronchioles, is lined with ciliated epithelium, with about 200 cilia on each epithelial cell. These cilia beat continually at a rate of 10 to 20 times per second by the mechanism explained, and the direc-tion of their “power stroke” is always toward the pharynx. That is, the cilia in the lungs beat upward, whereas those in the nose beat downward. This contin-ual beating causes the coat of mucus to flow slowly, at a velocity of a few millimeters per minute, toward the pharynx. Then the mucus and its entrapped particles are either swallowed or coughed to the exterior.
Cough Reflex
The bronchi and trachea are so sensitive to light touch that very slight amounts of foreign matter or other causes of irritation initiate the cough reflex. The larynx and carina (the point where the trachea divides into the bronchi) are especially sensitive, and the terminal bron-chioles and even the alveoli are sensitive to corrosive chemical stimuli such as sulfur dioxide gas or chlorine gas. Afferent nerve impulses pass from the respiratory passages mainly through the vagus nerves to the medulla of the brain. There, an automatic sequence of events is triggered by the neuronal circuits of the medulla, causing the following effect.
First, up to 2.5 liters of air are rapidly inspired. Second, the epiglottis closes, and the vocal cords shut tightly to entrap the air within the lungs. Third, the abdominal muscles contract forcefully, pushing against the diaphragm while other expiratory muscles, such as the internal intercostals, also contract forcefully. Conse-quently, the pressure in the lungs rises rapidly to as much as 100 mm Hg or more. Fourth, the vocal cords and the epiglottis suddenly open widely, so that air under this high pressure in the lungs explodesoutward. Indeed, sometimes this air is expelled at velocities ranging from 75 to 100 miles per hour. Importantly, the strong compression of the lungs collapses the bronchi and trachea by causing their noncartilaginous parts to invaginate inward, so that the exploding air actually passes through bronchial and tracheal slits. The rapidly moving air usually carries with it any foreign matter that is present in the bronchi or trachea.
Sneeze Reflex
The sneeze reflex is very much like the cough reflex, except that it applies to the nasal passageways instead of the lower respiratory passages. The initiating stimu-lus of the sneeze reflex is irritation in the nasal pas-sageways; the afferent impulses pass in the fifth cranial nerve to the medulla, where the reflex is triggered. A series of reactions similar to those for the cough reflex takes place; however, the uvula is depressed, so that large amounts of air pass rapidly through the nose, thus helping to clear the nasal passages of foreign matter.
Related Topics