Chapter: Medical Microbiology: An Introduction to Infectious Diseases: Cryptococcus, Histoplasma, Coccidioides, and Other Systemic Fungal Pathogens
Cryptococcosis : Clinical Aspects
CRYPTOCOCCOSIS : CLINICAL ASPECTS
MANIFESTATIONS
Meningitis is the most commonly recognized form of cryptococcal disease; it usually has a slow, insidious onset with relatively nonspecific findings until late in its course. Inter-mittent headache, irritability, dizziness, and difficulty with complex cerebral functions appear over weeks or months with no consistent pattern. Behavioral changes have been mistaken for psychoses. Fever is usually, but not invariably, present. Seizures, cranial nerve signs, and papilledema may appear later in the clinical course, as may dementia and decreased levels of consciousness. A more rapid course may be seen in AIDS patients, 5 to 15% of who become infected with C. neoformans.
Cryptococcal pneumonia is often asymptomatic or mild. Sputum production is mini-mal, and no findings are sufficiently specific to suggest the etiology. Skin and bone are the sites most frequently involved in disseminated disease; skin lesions are sometimes the presenting sign and are often remarkable for their lack of inflammation. The diagnosis is sometimes made when lesions are biopsied as suspected neoplasms.
DIAGNOSIS
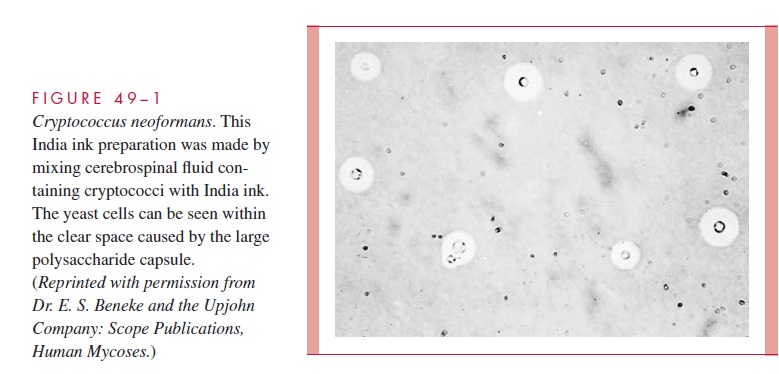
Typical cerebrospinal fluid (CSF) findings in cryptococcal meningitis are increased pres-sure, pleocytosis (usually 100 cells) with predominance of lymphocytes, and depression of glucose levels. In some cases, one or all of these findings may be absent, yet crypto-cocci are isolated on culture. Cryptococcal capsules are demonstrable in CSF in roughly 50% of cases by mixing centrifuged sediment with India ink and examining the mixture under the microscope (see Fig 49–1). Some experience is necessary to avoid confusion of lymphocytes with cryptococci. C. neoformans stains poorly or not at all with routine histo-logic stains; thus, it is easily missed unless special fungal stains are used.
In the isolation of C. neoformans, the volume of CSF sampled is important. The num-ber of organisms present may be small enough to require a substantial volume of fluid ( 30 mL) to yield a positive culture. If cryptococcosis is suspected and cultures are nega-tive, detection of the GXM polysaccharide antigen in the CSF or serum by latex agglutina-tion or enzyme immunoassay methods is recommended. These tests are very sensitive and specific, and their quantitation has prognostic significance. A rising antigen level indicates progression and a declining titer is a favorable sign.
TREATMENT
Amphotericin B (with or without flucytosine) or fluconazole is the usual treatment for systemic cryptococcal disease. Flucytosine use alone is limited by development of resistance during therapy. Although three fourths of persons with meningitis respond to treatment, a significant portion suffer relapses after antifungal therapy is stopped; many become chronic and require repeated courses of therapy. One half of those cured have some kind of residual neurologic damage.
Related Topics