Chapter: Essentials of Psychiatry: Eating Disorders
Bulimia Nervosa: Differential Diagnosis
Differential
Diagnosis
Bulimia
nervosa is not difficult to recognize if a full history is available. The
binge-eating/purging type of anorexia nervosa has much in common with bulimia
nervosa but is distinguished by the characteristic low body weight and, in
women, amenorrhea. Some individuals with atypical forms of depression overeat
when de-pressed; if the overeating meets the definition of a binge described
previously (i.e., a large amount of food is consumed with a sense of loss of
control) and if the binge-eating is followed by inappro-priate compensatory
behavior, occurs sufficiently frequently and is associated with over concern
regarding body shape and weight, an additional diagnosis of bulimia nervosa may
be warranted. Some individuals become nauseated and vomit when upset; this and
similar problems are probably not closely related to bulimia nervosa and should
be viewed as a somatoform disorder.
Many
individuals who believe they have bulimia nervosa have a symptom pattern that
fails to meet full diagnostic crite-ria because the frequency of their
binge-eating is less than twice a week or because what they view as a binge
does not contain an abnormally large amount of food. Individuals with these
characteristics fall into the broad and heterogeneous category of atypical
eating disorders. Binge-eating disorder, a category currently included in the
DSM-IV appendix B for categories that need additional research, is
characterized by recurrent binge-eating similar to that seen in bulimia nervosa
but without the regular occurrence of inappro-priate compensatory behavior.
Course and Natural History
Over
time, the symptoms of bulimia nervosa tend to improve although a substantial
fraction of individuals continue to engage in binge-eating and purging. On the
other hand, some controlled clinical trials have reported that structured forms
of psychother-apy have the potential to yield substantial and sustained
recovery in a significant fraction of patients who complete treatment. It is
not clear what factors are most predictive of good outcome, but those
individuals who cease binge-eating and purging com-pletely during treatment are
least likely to relapse.
Goals of Treatment
The goals
of the treatment of bulimia nervosa are straightfor-ward. The binge-eating and
inappropriate compensatory behav-iors should cease and self-esteem should
become more appropri-ately based on factors other than shape and weight.
Treatment
The power
struggles that often complicate the treatment proc-ess in anorexia nervosa
occur much less frequently in the treat-ment of patients with bulimia nervosa.
This is largely because the critical behavioral disturbances, binge-eating and
purging, are less egosyntonic and are more distressing to these patients. Most
bulimia nervosa patients who pursue treatment agree with the primary treatment
goals and wish to give up the core behavioral features of their illness.
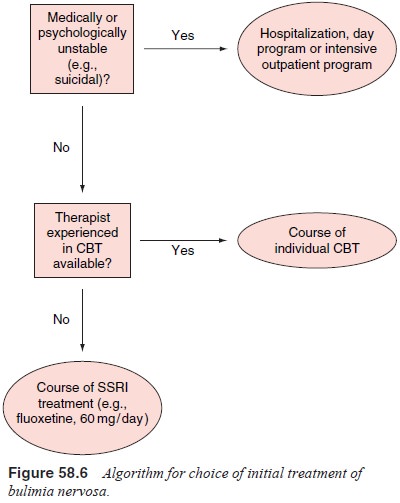
The
treatment of bulimia nervosa has received consider-able attention in recent
years and the efficacies of both psycho-therapy and medication have been
explored in numerous control-led studies (Figure 58.6). The form of
psychotherapy that has been examined most intensively is cognitive–behavioral
therapy, modeled on the therapy of the same type for depression.
Cogni-tive–behavioral therapy for bulimia nervosa concentrates on the distorted
ideas about weight and shape, on the rigid rules regard-ing food consumption
and the pressure to diet and on the events that trigger episodes of
binge-eating. The therapy is focused and highly structured and is usually
conducted in 3 to 6 months. Ap-proximately 25 to 50% of patients with bulimia
nervosa achieve abstinence from binge-eating and purging during a course of
cog-nitive–behavioral therapy and in most, this improvement appears to be
sustained. The most common form of cognitive–behavioral therapy is individual
treatment, although it can be given in either individual or group format. The
effect of cognitive–behavioral therapy is greater than that of supportive
psychotherapy and of interpersonal therapy, indicating that
cognitive–behavioral therapy should be the treatment of choice for bulimia
nervosa.
The other
commonly used mode of treatment that has been examined in bulimia nervosa is
the use of antidepressant medica-tion. This intervention was initially prompted
by the high rates of depression among patients with bulimia nervosa and has now
been tested in more than a dozen double-blind, placebo-control-led studies
using a wide variety of antidepressant medications. Active medication has been
consistently found to be superior to placebo, and although there have been no
large “head-to-head” comparisons between different antidepressants, most
antide-pressants appear to possess roughly similar antibulimic potency.
Fluoxetine at a dose of 60 mg/day is favored by many investiga-tors because it
has been studied in several large trials and ap-pears to be at least as
effective as, and better tolerated than, mostother alternatives. It is notable
that it has not been possible to link the effectiveness of antidepressant
treatment for bulimia nervosa to the pretreatment level of depression.
Depressed and nonde-pressed patients with bulimia nervosa respond equally well
in terms of their eating behavior to antidepressant medication.
Although
antidepressant medication is clearly superior to placebo in the treatment of
bulimia nervosa, several studies sug-gest that a course of a single
antidepressant medication is gener-ally inferior to a course of
cognitive–behavioral therapy. How-ever, patients who fail to respond adequately
to, or who relapse following a trial of psychotherapy, may still respond to
antide-pressant medication.
Special Features Influencing Treatment
A major
factor influencing the treatment of bulimia nervosa is the presence of other
significant psychiatric or medical illness. For example, it can be difficult
for individuals who are currently abusing drugs or alcohol to use the treatment
methods described, and many psychiatrists suggest that the substance abuse
needs to be addressed before the eating disorder can be effectively treated.
Other examples include the treatment of individuals with bulimia nervosa and
serious personality disturbance and those with insu-lin-dependent diabetes
mellitus who “purge” by omitting insulin doses. In treating such individuals,
the psychiatrist must decide which of the multiple problems must be first
addressed and may elect to tolerate a significant level of eating disorder to
confront more pressing disturbances
Refractory Patients
Although
psychotherapy and antidepressant medication are effective interventions for
many patients with bulimia nervosa, some individuals have little or no
response. There is no clearly es-tablished algorithm for the treatment of such
refractory patients. Alternative interventions that may prove useful include
other forms of psychotherapy and other medications such as opiate an-tagonists
and the serotonin agonist fenfluramine. Hospitalization should also be
considered as a way to normalize eating behavior, at least temporarily, and
perhaps to initiate a more effective out-patient treatment
Related Topics