Chapter: Medicine and surgery: Cardiovascular system
Atrial fibrillation - Atrial arrhythmias
Atrial fibrillation
Definition
Atrial fibrillation is a quivering of atrial myocardium resulting from disordered electrical and muscle activity.
Incidence
Common
Age
Increases with age: 1% in people aged 60 years and 5% over 70 years.
Sex
M > F
Aetiology
Causes may be divided into cardiac and systemic. Lone atrial fibrillation is when no structural or organic cause can be found.
┬Ę Cardiac: Atrial enlargement is a common mechanism for the onset of atrial fibrillation. Various cardiac and systemic conditions cause a chronic rise in atrial pressure and in time lead to atrial enlargement, e.g. ischaemic, hypertensive and rheumatic heart disease, mitral valve disease, cardiomyopathies and pulmonary disease.
┬Ę Systemic causes include thyrotoxicosis, alcohol and acute infections especially pneumonia.
Pathophysiology
Atrial fibrillation is the result of multiple reentrant circuits in the atria (see above). Since each of these numerous circuits have different cycle times, the result is a constant train of irregular impulses of various amplitude reaching the AV node, resulting in a very irregular ventricular response. The AV node blocks some of the transmissions, but an irregularly irregular pulse of between 100 and 160 per minute usually results. Atrial fibrillation may be paroxysmal with attacks lasting minutes to hours. Symptoms may arise if there is a high ventricular rate, in the elderly who depend on atrial function to achieve sufficient ventricular filling, or if there is associated significant cardiac damage. Abnormal atrial blood flow predisposes to thromboembolism.
Clinical features
Atrial fibrillation is often asymptomatic. Patients may present with palpitations, acute cardiac failure or the gradual onset of increasing shortness of breath. On examination there is an irregularly irregular pulse with varying pulse volume. There is also loss of the ŌĆśaŌĆÖ wave of the JVP.
Investigations
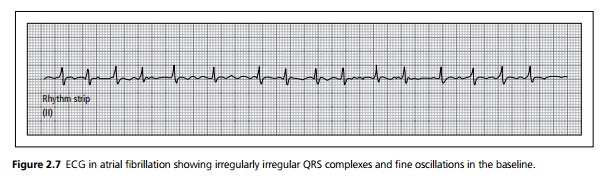
ECG shows fine irregular oscillations of the base line, with a QRS totally irregular in timing normally at a rate of between 100 and 160 bpm (see Fig. 2.7).
Thyroid function tests should be performed in all patients. In acute atrial fibrillation, underlying ischaemia such as a recent myocardial infarction or unstable angina should be excluded.
Management
Restoration of sinus rhythm may be achieved with synchronised DC cardioversion or by use of amiodarone or other drugs. DC cardioversion has a high relapse rate. The longer the atrial fibrillation has been present, the less the likelihood of restoring sinus rhythm.
Maintenance of sinus rhythm may be achieved with anti-arrhythmic drugs, but long-term use of amiodarone has significant side effects. Digoxin does not prevent recurrence.
Control of the ventricular rate is achieved with drugs such as digoxin, calcium channel blockers and/or ╬▓-blockers.
Warfarin anticoagulation is used in patients over the age of 65 years and in those at increased risk of thromboembolism including presence of hypertension, valve disease and left ventricular dysfunction. In younger patients without other risk factors aspirin may be used as an alternative. Anticoagulation is also indicated for at least 1 month preceding and post-DC cardioversion.
Related Topics