Chapter: Essentials of Psychiatry: The Cultural Context of Clinical Assessment
Working with Interpreters and Culture-brokers
Working with Interpreters and
Culture-brokers
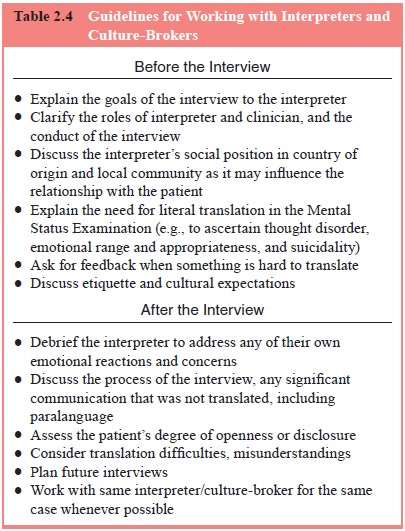
A key skill which has not been addressed in many
training pro-grams concerns how to work with interpreters (Table 2.4). In the
absence of familiarity with this technique and quality assur-ance standards
insisting on appropriate use of interpreters, many clinicians simply try to
avoid the situation, relying on patients’ sometimes limited command of the
clinician’s language. This is unfortunate and may lead to errors in diagnosis
and management as well as the failure to engage and help many patients.
There are several models of working with
interpreters (Westermeyer, 1989). Medical interpreters have adopted a code of
ethics and model of working that owes much to forensic and political
interpreting. Their goal is to provide accurate, complete and literal
translation of the statements of patient and physician. This model tends to
portray the interpreter as providing a trans-parent window or conduit of
communication between clinician and patient. In this approach, the clinician
addresses the patient directly as though the interpreter is not present. The
interpreter may speak in the first person for the patient and for the clinician
alternately. The model assumes that it is possible to achieve com-plete and
accurate translation of message in both directions and treats the interpersonal
triad of doctor–interpreter–patient as if it was a dyad. To do so assumes that
the interpreter does not have an independent relationship with patient or
clinician. Of course, this is certainly not the case in any clinical encounter
that goes on for a time or involves repeated meetings. Indeed, at the level of
transference it is never the case because the mere presence of another person
immediately evokes distinctive thoughts, feelings
Table 2.4 Guidelines
for Working with Interpreters and Culture-Brokers
Before the
Interview
·
Explain the goals of the interview to the interpreter
·
Clarify the roles of interpreter and clinician, and the
conduct of the interview
·
Discuss the interpreter’s social position in country of
origin and local community as it may influence the relationship with the
patient
·
Explain the need for literal translation in the Mental
Status Examination (e.g., to ascertain thought disorder, emotional range and
appropriateness, and suicidality)
·
Ask for feedback when something is hard to translate
·
Discuss etiquette and cultural expectations
After the
Interview
·
Debrief the interpreter to address any of their own
emotional reactions and concerns
·
Discuss the process of the interview, any significant
communication that was not translated, including paralanguage
·
Assess the patient’s degree of openness or disclosure
·
Consider translation difficulties, misunderstandings
·
Plan future interviews
·
Work with same interpreter/culture-broker for the same case
whenever possible
and fantasies. Then too, the presence of the
interpreter inevitably changes a dyad into a triadic social system with its own
complex interpersonal dynamics. These dynamics are complicated by the
ethnocultural background of the interpreter and his or her own cultural
assumptions.
The very idea of literal translation is also
problematic. Across languages, words and phrases with similar denotation often
have different sets of connotations. Every translation, there-fore, is an interpretation
that emphasizes some potential mean-ings while muting or eliding others.
Interpreters tend to smoothe out fragmentary, incomplete, or incoherent
statements and so may mask thought disorder or other idiosyncrasies of speech
with diagnostic relevance. The clinician needs to understand the choice of
alternatives made by the interpreter in order to appre-ciate the connotations
of the patient’s words and to convey his or her own nuanced meanings. These
requirements place much higher demands on interpreting in mental health setting
than in other medical or legal settings.
A slightly different model views the interpreter as
a “go-between”. In this approach, the interpreter takes turns interact-ing with
clinician and patient to clarify what is being said and to find a means of
conveying it. This model acknowledges the interpreter as an active intermediary
and allows the interpreter some autonomy. The sequential dyadic interaction
puts greater time and distance between clinician and patient. This demands that
the interpreter have a high degree of clinical knowledge and interpersonal
skill, which is possible when the interpreter has been trained as a clinician.
Taking this autonomy further, the in-terpreter may be viewed as a cotherapist.
In this approach, the interpreter with clinical skills develops his or her own
working alliance with the patient. The interpreter may respond independ-ently
to the patient and initiate interventions. This sometimes happens because of
language barriers, when patients may contact the interpreter to ask for help
with practical issues.
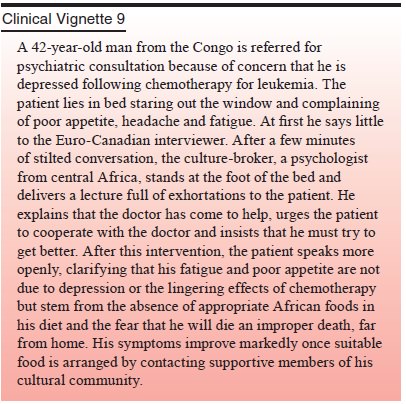
Given the complexities of interpreting, we prefer
to view the interpreter as a culture-broker who works to provide both the
patient and the clinician with the cultural context needed to understand each
other’s meanings. To do this, the interpreter must understand something of the
perspectives, cultural back-ground and social positions of both patient and
clinician and appreciate the goals of the clinical task. Based on this
knowl-edge, the culture-broker can enhance patient and clinician un-derstanding
of each other and can help negotiate compromises when there are widely
divergent understandings of a problem and its solutions.
Despite increasing recognition of the importance of
ad-equate interpretation, many clinicians or institutions use lay in-terpreters
who are directly available at no cost, usually family members (even children)
or other workers within the institution. Except in emergency situations, this
practice should be avoided because it exerts a strong censorship on what may be
disclosed in the encounter and because it may damage relationships that are
very important to the patient by transgressing certain social and familial
taboos.
Both interpreters and culture brokers need training
to per-form competently, and clinicians need training, in turn, to work with
these allied professionals. The clinician must take a sys-temic approach,
understanding the other people in the room as part of an interactional system.
Clinicians must also understand the interpreter’s position in the larger
community. Some of this training can go on when clinicians have an opportunity
to work repeatedly with the same interpreters, who thus become part of a
treatment team.
Related Topics