Chapter: Essentials of Psychiatry: The Cultural Context of Clinical Assessment
Illness Explanations and Help-seeking
Illness Explanations and
Help-seeking
The second major dimension of the cultural
formulation concerns cultural explanations of symptoms and illness. Cultures
provide systems of diagnosis and treatment of illness and affliction that may
influence patients’ experience of illness and help-seeking behavior. People
label and interpret their distress based on these systems of knowledge, which
they share with others around them. Much
Table
2.2 Explanatory Model Interview
1. What do you
call your problem?
2. What causes
your problem?
3. Why do you
think it started when it did?
4. How does it
work?
5. What is going
on in your body?
6. What kind of
treatment do you think would be best for this problem?
7. How has this
problem affected your life?
8. What frightens
or concerns you most about this problem or treatment?
research in medical anthropology has developed the
idea of ex-planatory models, which may include accounts of causality,
mecha-nism or process, course, appropriate treatment, expected outcome and
consequences. Not all of this knowledge is related directly to personal
experience – much of it resides in cultural knowledge and practices carried by
others. Hence, understanding the cultural meanings of symptoms and behavior may
require interviews with other people in the patient’s family, entourage, or
community.
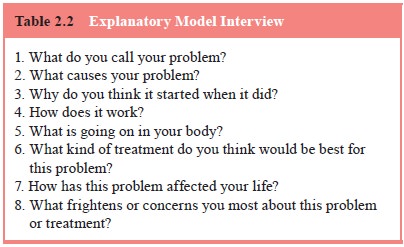
Table 2.2 provides questions for eliciting
patients’ explan-atory models. These questions should be modified based on the
patient’s responses. For example, the origins of problems may be located not in
the body but in the workings of the mind, the family, the community, the realms
of ancestors or spirits, or in mythological accounts that explain the social
and moral order.
In many cases, particularly with acute illness,
patients may not have well-developed explanatory models. Instead, they reason
by analogy on the basis of past experiences of their own or other prominent
prototypes encountered in family, friends, or mass media. Once an explanatory
model is evoked in conver-sation, however, patients may give formulaic accounts
that ac-cord with that cultural model or script. Therefore, to obtain more
complete information about the cognitive and social factors that are actually
influencing the patients’ illness experience and be-havior, it is useful to
begin with an open-ended interview that simply aims to reconstruct the events
surrounding symptoms and the illness experience. This will reveal idiosyncratic
temporal patterns of contiguity and association that may not fit any explicit
cultural model. Following this, the clinician can ask about proto-types (Have
you ever had anything like this before? Has anyone you know ever had anything
like this before?) This will uncover salient models of illness that may shape
illness experience and be used to reason analogically about the current
episode. Finally, it is important to inquire into explicit cultural models
using the sorts of questions devised for the explanatory model interview.
The ethnomedical systems described in
anthropological texts often are idealized and complex portraits pieced together
by working with cultural experts. In clinical practice, patients usually have
only partial or fragmentary knowledge of the tradi-tional explanations and
treatment for their problem. Depending on the knowledge and attitudes of family
and kin, and on the availability of practitioners of traditional medical
systems, pa-tients may be influenced by larger cultural systems to which they
themselves do not fully subscribe.
In everyday life, people use culturally prescribed
idioms to discuss their problems. These cultural idioms of distress cut across
specific diagnostic categories. They may be used to talk about ordinary
problems as well as to shape the expression of distress associated with major
psychiatric disorders. For exam-ple, many cultures have notions of “nerves” (in
Spanish, nervios), which signal
emotional distress that may range from mild upset with life events to disabling
anxiety or psychosis. Appendix I of DSM-IV-TR provides a list of some common
idioms of distress. The same appendix also lists some well-described culture
bound syndromes, culturally distinctive clusters of symptoms that may be of
pathological significance. Many culture-specific terms, however, do not refer
to syndromes or idioms of distress but are actually symptoms or illness
attributions that reference folk models of causality. For example, susto, a term used in Central and South
America, attributes a wide range of bodily symptoms and diseases (including
infectious diseases and congenital mal-formations) to the damaging effects of
sudden fright.
Many cultural idioms of distress use bodily
metaphors for experience. In seeking medical help, patients usually try to
present the sort of problems they believe the clinician is com-petent to treat.
Consequently, in biomedical settings patients tend to emphasize physical
symptoms. This pattern of clinical presentation combined with the wide currency
of somatic idioms of distress has led to a characterization of many
ethnocultural groups as prone to somatize their distress (Kirmayer, 2001). The
social stigma commonly associated with psychiatric symptoms and disorders, as
well as with substance abuse, antisocial behav-ior and various other behaviors
also may prevent patients from acknowledging such problems and events. However,
with clear communication and a respectful stance, the clinician may be able to
build sufficient trust over time for patients to disclose shame-ful or
potentially stigmatizing information.
Similarly, people commonly use multiple remedies or
con-sult various healers for their symptoms, and may be reluctant to disclose
treatments they think the clinician will not understand or accept. They may
also omit mention of preparations they view as “natural” or as foods and hence
not included under the rubric of medications or drugs. Commonly used remedies
like ginseng, St John’s Wort and Gingko
biloba have significant effects on pharmacokinetics and drug metabolism and
are, therefore, important for their potential impact on physiology as well as
their role in patients’ belief systems and sense of control over their illness.
A nonjudgmental inquiry by the clinician willenable patients more freely to
discuss their use of traditional and alternative treatments.
Related Topics