Chapter: Clinical Cases in Anesthesia : Thoracic Trauma
When should traumatic thoracic aortic injury be suspected and how is the diagnosis made?
When
should traumatic thoracic aortic injury be suspected and how is the diagnosis
made?
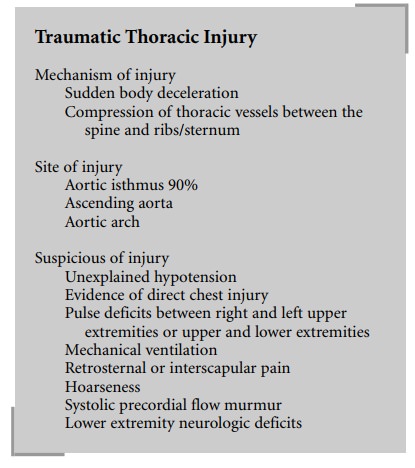
Traumatic thoracic cardiovascular injury is a
potentially lethal sequela of chest trauma carrying an almost 80% mortality in
the first hour following the trauma. It should be suspected in every patient
with blunt chest trauma. Although the majority of patients sustain the injury
from sudden body deceleration after a motor vehicle accident or fall, other
mechanisms such as sudden compression of the thoracic vessels between the spine
and sternum or ribs can also produce this injury. In almost 90% of instances,
the aorta is injured at the isthmus, the junction of its free and fixed
portions. Injuries to the ascending portion and the aortic arch are much less
frequent than isthmic injuries. A history of violent deceleration, ejection of
an unrestrained passenger from the vehicle, death of anyone involved in the
accident, a motor vehicle/pedestrian or bicyclist collision, or the pres-ence
of high-impact injuries such as diaphragmatic rupture or mesenteric tear should
enhance the suspicion for this injury. Additionally, chest trauma patients who
develop unexplained hypotension, external signs of direct chest injury, pulse
deficits between right and left arms or between upper and lower extremities,
requirement for mechanical ventilation, presence of retrosternal or
interscapular pain, hoarseness, systolic precordial flow murmur, or lower
extremity neurologic deficits may also have an aortic injury. All patients
should have a chest radiograph following chest trauma. Only 20–30% of instances
of mediastinal widening on chest films are associated with thoracic aortic
injury. Other chest radiographic findings suggestive of aortic injury are
blurred aortic contours, wide paraspinal interface, opaci-fied pulmonary
window, broad paratracheal stripe, displaced left mainstem bronchus, rightward
deviation of the esopha-gus and trachea, and left hemothorax.
Aortography is the gold standard for the
diagnosis of traumatic aortic injury. However, recent improvements in CT and
ultrasound technologies permit reliable noninvasive diagnosis in the majority
of patients. Contrast-enhanced spi-ral CT and multiplanar TEE are highly
accurate and have substantially decreased the need for aortography. These two
techniques are equally capable of diagnosing subadventitial aortic injuries
which require surgical intervention. Lesions of the intima and media, which can
be treated conservatively but which may later result in a pseudoaneurysm, and
concomitant BCI are much more likely to be detected by TEE than by CT. The high
diagnostic accuracy of TEE is valuable for both patients and anesthesiologists.
Most patients who are admitted do not have major aortic tears, thus their
hemodynamic abnormality generally originates from other injuries, such as to
the spleen or liver, which require immedi-ate surgery without time for further
evaluation of the chest. Intraoperative TEE in these instances eliminates the
uncer-tainty about the presence of this injury that was common in the past, and
permits appropriate intervention for nonaortic injuries while the diagnosis is
made by the anesthesiologist. Aortic branch injuries, however, are difficult to
be detected by TEE; angiography provides more accurate diagnosis for these
injuries. TEE is also contraindicated in patients with sus-pected esophageal
injuries. These patients frequently mani-fest bloody nasogastric tube drainage,
severe facial trauma, unstable cervical spine injuries, and pneumoperitoneum.
Although TEE is a useful technique in stable patients with mediastinal
widening, flail chest, or pulmonary contusion, contrast-enhanced spiral CT
appears to be the method of choice for definitive diagnosis.
The TEE findings of traumatic thoracic aortic
injury include dilated aortic isthmus with abnormal contour, acute false
aneurysm formation or an intraluminal medial flap associated with
subadventitial disruption or both, a mobile image appended to the thoracic
aortic wall consistent with an intimal tear or a mural thrombus, or a
crescentic or circumferential thickening of the aortic wall suggesting the
presence of intramural hematoma. In addition, a traumatic hemomediastinum
should be considered if the distance between the esophageal probe and the
anteromedial wall of the aortic isthmus is >3 mm or there is blood between
the posterolateral aortic wall and the left visceral pleura. A left-sided
hemothorax can be detected if there is blood between the left lung and the
thoracic wall.
The CT findings of traumatic aortic injury
include: polypoid or linear intraluminal areas of low attenuation sug-gesting
clot or medial flap, false aneurysm, irregular aortic wall or contour,
pseudo-coarctation, intramural hematoma, and aortic dissection.
Related Topics