Chapter: Clinical Cases in Anesthesia : Thoracic Trauma
How are traumatic pneumothorax and/or hemothorax managed in a patient undergoing laparotomy for splenic injury?
How are
traumatic pneumothorax and/or hemothorax managed in a patient undergoing
laparotomy for splenic injury?
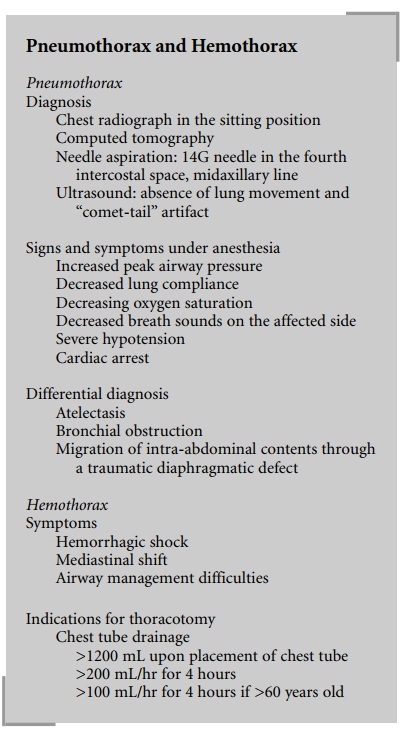
Pneumothorax and/or hemothorax are the most
frequent consequences of chest injury and require timely recognition and
treatment. Concerns about exacerbating spine injuries or producing adverse
hemodynamic changes preclude obtain-ing a chest radiograph in the sitting
position, which is required for the diagnosis of a pneumothorax and
recogni-tion of the magnitude of a hemothorax. For these reasons, while supine
chest radiographs are obtained routinely in all major trauma patients,
additional measures may be neces-sary to diagnose pneumothorax and hemothorax
when their presence is suspected. Computed tomography (CT) of the chest is
highly specific for this purpose, and even a small amount of air in the pleural
cavity can be recognized by this method. Unfortunately, in some instances a
preoperatively undiagnosed pneumothorax may enlarge during surgery for
associated injuries, and result in severe hemodynamic and oxygenation
abnormalities and potentially death if not recognized in time.
The clinical signs and symptoms of pneumothorax
in anesthetized patients receiving positive-pressure ventilation include
elevation of peak airway pressure, decreased lung compliance, decreasing oxygen
saturation, decreased breath sounds on the affected side and, in extremis,
severe hypoten-sion, and even cardiac arrest. A chest radiograph can provide
the diagnosis even in the supine position if there is a large amount of
intrapleural air; however it may be difficult or impossible to obtain during
emergency surgery.
Without a radiologically confirmed diagnosis,
placement of a 14G needle between the fourth and fifth ribs (the fourth
intercostal space) in the midaxillary line, the thinnest region of the chest
wall even in obese patients, may be indicated in unstable patients.
Nevertheless, atelectasis, bronchial obstruc-tion, or migration of
intra-abdominal contents into the chest through a traumatic diaphragmatic defect
can mimic the clinical findings of pneumothorax and lead to chest tube
placement that is not indicated. Recently, the sonographic diagnosis of
pneumothorax has gained some recognition.
Normally, when the lung is imaged by a 3.5–7.5 MHz
ultrasound probe, it moves beneath the chest wall during each inspiration, and
so-called comet-tail artifacts, multi-ple echodense spots at the surface of the
lungs, appear in the image. In the presence of pneumothorax, neither lung
movement (sliding) nor comet-tail artifacts can be observed in the ultrasound
image.
Hemothorax may also cause hemorrhagic shock,
medi-astinal shift, and airway management difficulties. The volume and rate of
blood drained via a chest tube determine the necessity of thoracotomy. Drainage
of >1,200 mL of blood upon placement of a chest tube, and/or continuing
drainage of >200 mL/hour for 4 hours, or >100 mL/hr for 4 hours in
patients older than 60 years, are indications for thoracotomy. Other
indications for emergency surgery include significant hypotension and/or
tachycardia, persistence of “white lung” on the chest radiograph in the
presence of a properly placed chest tube, difficulty of ventilation,
pericardial tamponade, massive air leak from the chest tube, and cardiac or
great vessel injury.
Related Topics