Chapter: Clinical Cases in Anesthesia : Thoracic Trauma
What are the management options for flail chest and pulmonary contusion?
What are
the management options for flail chest and pulmonary contusion?
Diagnosis
The presence of a flail segment obviously
suggests an underlying pulmonary contusion, but if the patient is breathing
rapidly and shallowly, this sign may not be evident. It should be emphasized,
however, that neither the extent of the flail nor the number of ribs fractured
accurately predicts respiratory failure. Chest wall bruising, rib cage
deformities, and crepitus and/or pain during palpation of the thorax should
suggest the presence of rib fractures or dislocation even in the presence of a
normal chest radiograph. Cartilaginous injuries and fractures of poorly
calcified ribs may not be detected by chest radio-graph. The initial film often
does not show an underlying lung injury since pulmonary edema appears late. If
present, a focal infiltrate beneath an area of multiple rib fractures makes the
diagnosis of pulmonary contusion. Clinical signs such as dyspnea, tachypnea,
intercostal muscle retrac-tion, and the use of accessory muscles of respiration
should suggest underlying lung pathology. Monitoring with pulse oximetry in the
initial stage is useful only if the patient is breathing room air; supplemental
oxygen administration may mask inadequate ventilation, delaying the diagnosis
and maneuvers that restore FRC and lung compliance toward normal. Likewise,
arterial blood gases measured with the patient breathing room air may be
useful. Of course, managing these patients without supplemental oxygen
necessitates direct observation by a physician or qualified person. The usual
pattern is a progressive decrease in arte-rial oxygen (PaO2) and
increase in carbon dioxide (PaCO2) tensions resulting in a decrease
in pH (respiratory acidosis). Although arterial hypoxemia may precede
radiographic abnormalities, it may not reflect the size of the contusion
because of restriction of blood flow to the injured lung by hypoxic pulmonary
vasoconstriction. A PaO2/FIO2 <300 after
the initial resuscitation phase is considered a risk factor for the development
of subsequent acute respiratory failure. Quantifying the contusion volume with
a chest radiograph, and preferably with a CT scan, may have a prognostic value
for identifying the patient who will develop acute respira-tory distress
syndrome (ARDS). Patients with contusion volumes greater than 20% of total lung
volume are more likely to develop ARDS and pneumonia.
Treatment
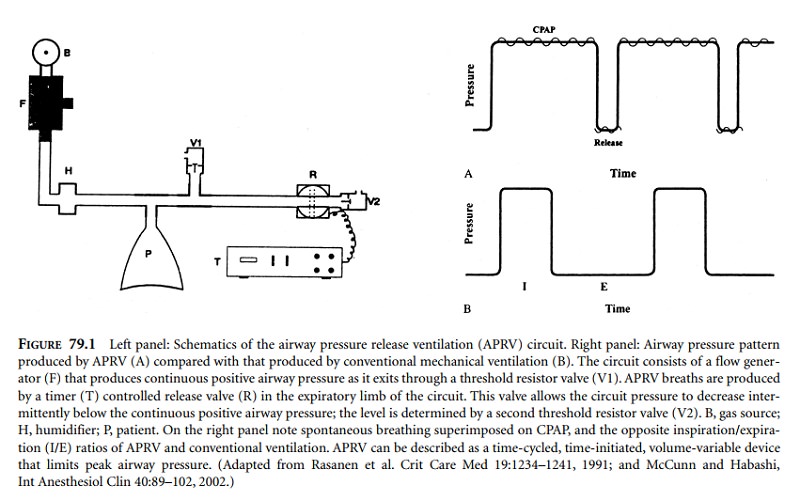
Early treatment is of utmost importance. A delay of even a few hours may result in progression of underlying lung pathology, with increasing morbidity and mortality. The goal is to decrease elastic recoil and the work of breathing, and to improve arterial blood gases without adverse hemodynamic effects. In patients without acute respiratory failure or associated injuries requiring tracheal intubation this can best be accomplished by continuous positive airway pressure (CPAP) of 10–15 cm H2O applied by face mask. The routine use of early tracheal intubation and mechanical ventilation with alveolar recruitment maneuvers, the usual practice before 1975, has fallen into disfavor because of an unacceptably high incidence of tracheobronchitis and pneumonia leading to sepsis, multiorgan failure, and death. At present, except in instances when tracheal intubation and mechanical ventilation are necessary (PaO2 <60 mmHg in room air, or <80 mmHg with supplemental oxygen, and conditions other than thoracic injury), the vast majority of patients do well with CPAP. When impending respiratory failure indicates tracheal intu-bation, airway pressure release ventilation (APRV) may be a reasonable choice. With this mode of ventilation in the spon-taneously breathing patient, CPAP is intermittently decreased for short periods with the device shown in Figure 79.1. In other words, spontaneous breathing is superimposed on mechanical ventilation. In addition to decreased work of breathing, the advantages of this technique over controlled mechanical ventilation are improved ventilation/perfusion (V/Q) matching, increased systemic blood flow, lower sedation requirement, greater oxygen delivery, and shorter periods of intubation.
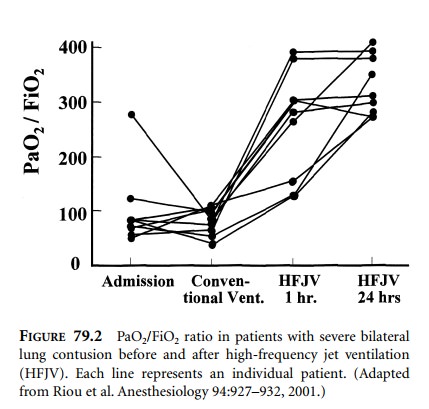
In patients with severe life-threatening
unilateral pul-monary contusion unresponsive to mechanical ventilation or APRV,
differential lung ventilation via a double-lumen endobronchial tube should be
considered. In bilateral severe contusions with life-threatening hypoxemia,
high-frequency jet ventilation has been shown to improve systemic oxygenation
effectively (Figure 79.2). This mode of ventilation may also improve depressed
cardiac function caused by concomitant myocardial contusion or ischemia.
Irrespective of the mode of ventilation,
effective removal of tracheobronchial secretions has a significant effect on
outcome. Likewise, monitoring with pulse oximetry, an arterial line and, when
indicated, a pulmonary artery catheter is important. The pulmonary artery
catheter not only guides fluid management, which should be adjusted to the
mini-mum consistent with adequate end-organ perfusion, but it also helps in
ventilatory management, as it permits calcula-tion of oxygen delivery and
intrapulmonary shunt fraction and thus helps to adjust the optimal level of
CPAP.
Supplemental oxygen should be administered
judiciously in order to permit the acquisition of maximal information from the
initial oxyhemoglobin saturation with pulse oximetry or arterial blood
analysis, as well as to avoid its detrimental effects, such as absorption
atelectasis, interfer-ence with hypoxic pulmonary vasoconstriction in damaged
lung regions, decreased mucociliary clearance, free radical formation, and
decreased surfactant production.
Overzealous fluid infusion may result in an
increase in the size of the lung contusion and a decrease in PaO2.
Although it is possible to remove excess fluid with diuret-ics, their use is
associated with electrolyte abnormalities, cardiac dysrhythmias, and
hypovolemia. At least during initial resuscitation, the type of fluid used does
not seem to affect outcome. Crystalloid solutions are favored because they are
less expensive. In the presence of concomitant blunt cardiac injury, the
complications of pulmonary contusion can easily confuse the clinical picture.
In this situation, transesophageal echocardiography (TEE) or, if TEE is not
available, pulmonary artery and wedge pressures are the best guides to fluid
management.
Continuous epidural analgesia is the best pain
manage-ment technique available for blunt chest trauma. It improves lung
function and thus decreases overall morbidity. Other modalities, such as
parenteral opioids, are not nearly as effec-tive, while multiple intercostal
blocks are labor-intensive and short-lasting, and thus must be repeated at
least twice a day. Continuous thoracic paravertebral block has been described
but awaits further clinical evaluation.
Related Topics