Chapter: Essentials of Psychiatry: The Psychiatric Interview: Settings and Techniques
What Is the Diagnosis?
What Is the Diagnosis?
In psychiatry, as in the rest of medicine,
descriptive information about signs, symptoms and course over time is used to
assign a diagnosis to the presenting problem. Not all psychiatric diag-noses
have well-established validity, but most convey knowl-edge of prognosis,
comorbidity, treatment response, occurrence in family members, or associated
biological or psychological findings (Tischler, 1987). Even in the case of
poorly understood entities, our present system of diagnosis using specific
criteria maximizes uniformity in the description and naming of psychi-atric
disorders.
One important implication of diagnoses is whether
there may be reduced plasticity of brain functioning due to anatomi-cal or
physiological abnormalities. Symptoms, deficits and be-haviors which stem from
such abnormalities vary less in re-sponse to environmental and motivational
factors than those behaviors which arise in the context of normal brain
function. For example, mood swings in a patient with bipolar disorder, a
condition for which there is strong evidence of a biological–ge-netic etiology,
typically recur at regular time intervals, often independently of the patient’s
life situation. By contrast, mood swings in a patient with narcissistic
personality disorder are much more likely to be triggered by interactions with
other people. Furthermore, when brain function is impaired, biologi-cal
treatments are more likely to be necessary, and verbal, in-terpersonal, or
environmental interventions are less likely to be sufficient. Thus, the
likelihood of altered brain function has major implications for understanding
and treating the patient’s problems.
Although the question of brain abnormalities is
basic to psychiatric triaging, we do not yet have a clearcut biological
etiology for any disorder outside of those historically classi-fied as
“organic”. Standard laboratory studies (such as brain imaging or
electroencephalography) are not generally diag-nostic of psychopathology;
however, there is research-based evidence of altered brain function in many
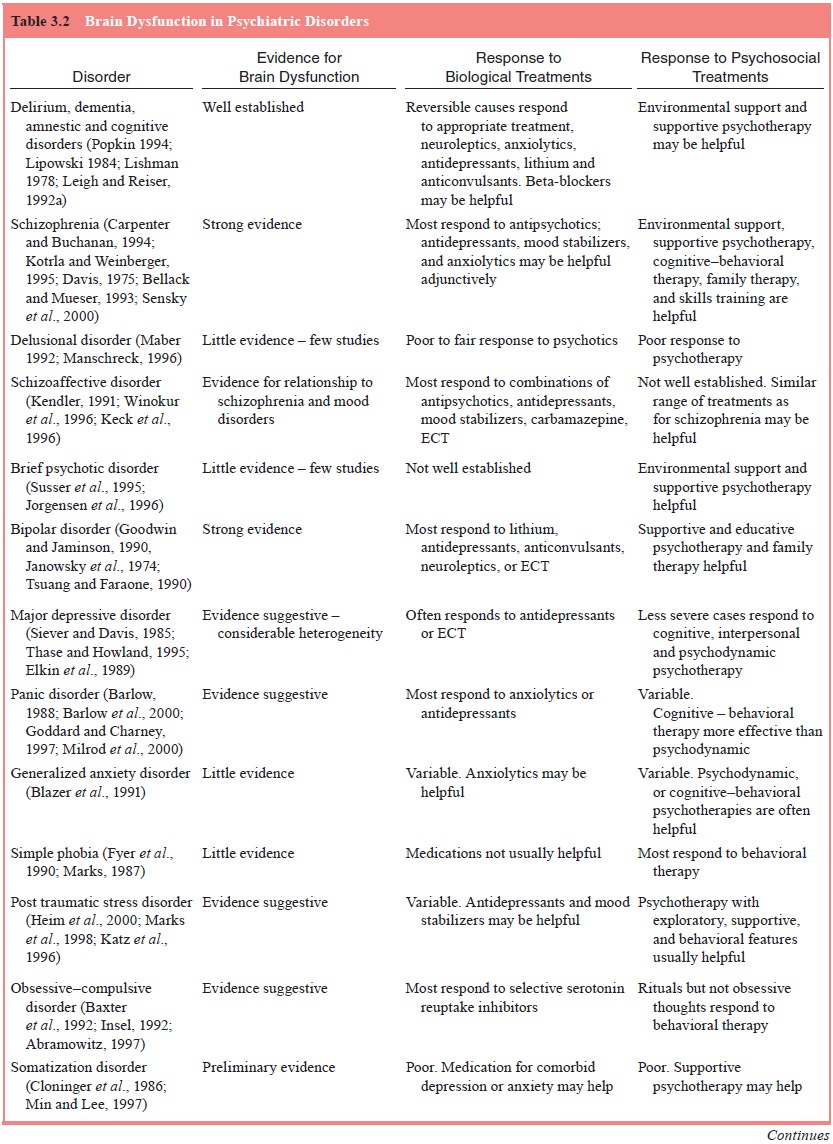
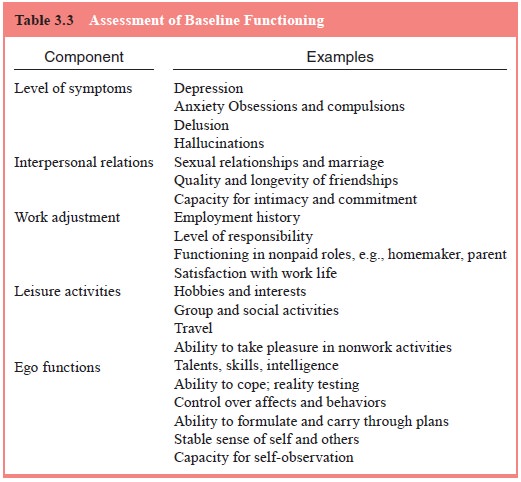
psychiatric dis-orders. Table 3.2 presents an overview of the current state of
knowledge of brain abnormalities in psychiatric disorders, along with known
responses to biological and psychosocial treatments.
What Is the Patient’s Baseline Level of Functioning?
Determining what the patient has been like in
his/her best or most usual state is a vital part of the assessment. This
informa-tion allows the interviewer to gauge when the patient became ill, and
how he/she is different when ill versus well. Environ-mental, biological and
psychological factors that contribute to low baseline levels of functioning may
also predispose a patient to the development of psychiatric disorders. Thus,
in-formation about baseline functioning provides clues about the patient’s areas
of vulnerability to future illness as well as his/ her capacity to benefit from
treatment. It is also an important guide to realistic goals and expectations
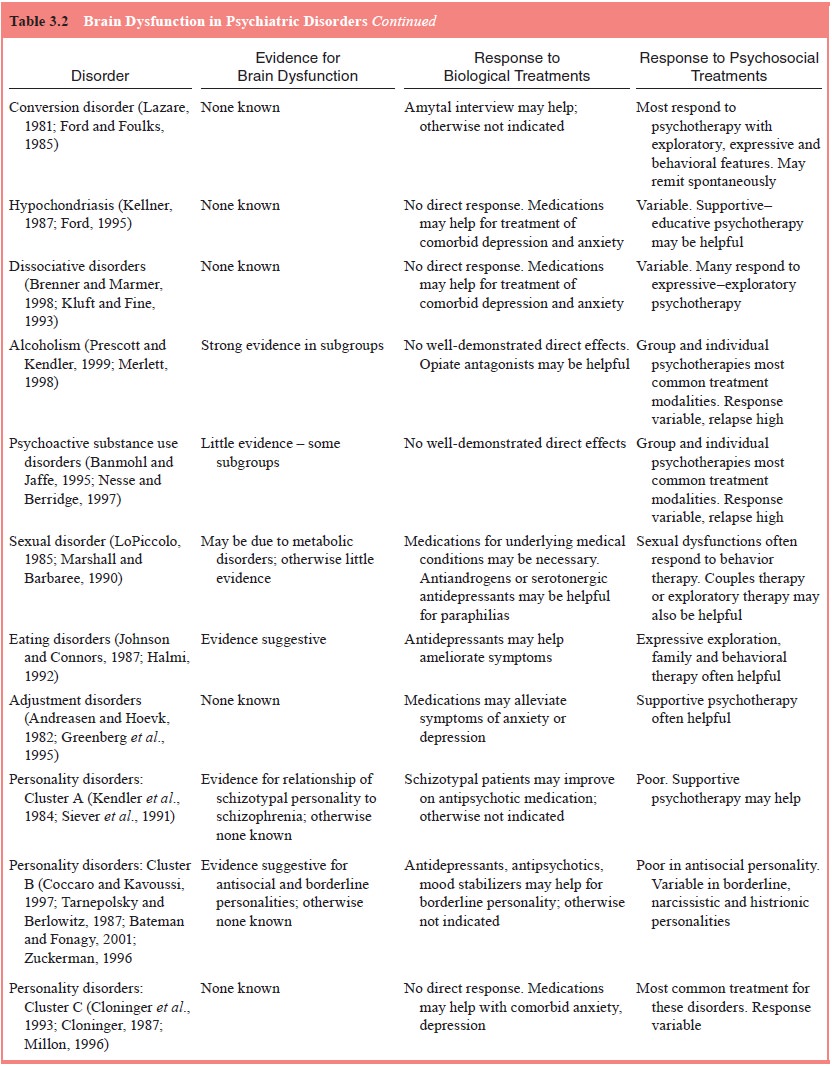
for such treatment. Table 3.3 lists major components of functioning with
examples of elements of each.
What Environmental Factors Contribute to the Disorder?
Environmental contributions to the presenting
problem are factors external to the patient. They may be acute events which
precipitate illness, or longstanding factors which increase general
vulnerability. Loss, change and traumatic events are very common acute
precipitants (Paykel, 1978). Longstand-ing environmental stressors may
predispose the patient to the development of illness and may also worsen the
outlook for recovery.
It is important to identify adverse environmental
influ-ences which can be modified, and to help the patient or family make
necessary changes. For example, a patient with recurrent paranoid psychosis
needed yearly hospitalization as long as she worked in an office with many
other people. However, she no longer suffered severe relapses when she was
helped to find work which she could do in her own home. However, even
irreversible precipitants, such as death of a loved one, must be identified and
dealt with in the treatment plan.
What Biological Factors Contribute to the Disorder?
Biological factors may contribute to psychiatric
disorders directly by their effects on the central nervous system and
indirectly through the effects of pain, disability, or social stigma. Thus,
biological factors must be assessed through both the psychiatric history and
diagnosis, and the general medical history.
Biological factors affecting the central nervous
system may be genetic, prenatal, perinatal, or postnatal. There is strong
evidence of genetic contributions to schizophrenia, bipolar dis-order and
alcoholism, among others (Carpenter and Buchanan, 1994; Jorgensen et al., 1996; Kluft and Fine, 1993);
conditions such as maternal substance abuse or intrauterine infections
mayaffect fetal brain development; birth complications may cause cerebral
hypoxia with resultant brain damage. In postnatal life, the entire range of
diseases which affect the brain may alter men-tal function and behavior, as may
exposure to toxins at work, in the environment, and through substance abuse. In
addition, medical conditions which do not directly affect brain functioning may
have profound effects on the patient’s state of mind and behavior.
Biological factors may both predispose to and
precipi-tate episodes of illness. Thus, a patient with a genetic vulner-ability
to schizophrenic illness may have an episode of acute psychosis precipitated by
heavy cocaine use. Similarly, a pa-tient with borderline low intellectual capacity
due to hypoxia at birth may have marginal ability to care for herself. An
accident resulting in a fractured arm might overwhelm this person’s coping
capacity and precipitate a severe adjustment disorder.
What Psychological Factors Contribute to the Disorder?
Psychological factors are mental traits which the
patient brings to life situations. While they interact with social and
environmen-tal factors, they are intrinsic to the individual, and not readily
changed by outside influences.
Psychological factors predisposing to illness
include both general and focal deficits in coping adaptability. General
defi-cits encompass the entire range of ego functioning, including poor reality
testing, rigid or maladaptive psychological defense mechanisms, low ability to
tolerate and contain affects, impulsiv-ity, poorly formed or unstable sense of
self, low self-esteem and hostile, distant, or dependent relationships with
others (Valliant, 1977). Patients with such deficits generally meet diagnostic
crite-ria for one or more personality disorders and are at increased risk for
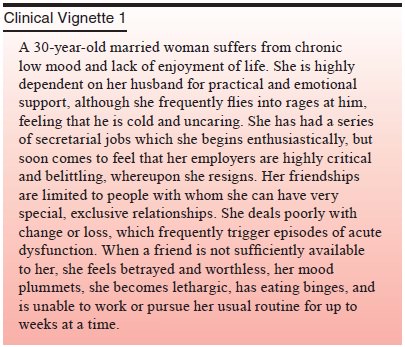
episodes of acute psychiatric illness. An example of general deficits in
psychological functioning is illustrated by the follow-ing case.
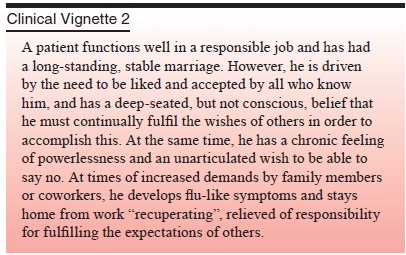
Focal psychological issues may also contribute to
mental disorders. These issues, which typically involve conflicts between
opposing motivations, may affect the patient in certain specific areas of
function or life situations, leaving other broad areas of function intact
(Nemiah, 1961a). Such conflicts are most likely to cause maladaptive behaviors
or symptoms when the patient is not clearly aware of them.
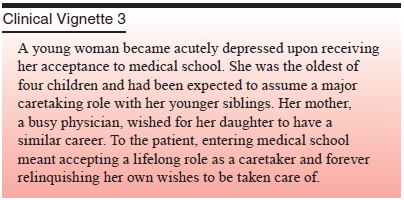
The meaning of an event in the context of the
patient’s life course is another focal issue which may contribute to illness.
What Is the Patient’s Motivation and Capacity for Treatment?
Whatever the physician’s view of the presenting
problem, the patient’s wishes and capacities are a major determinant of
treat-ment choice (Lazare et al.,
1975). Some patients seek relief of symptoms; some wish to change their
behavior or the nature of their relationships; some want to understand
themselves better. Patients may wish to talk or to receive medication or
instructions.
The patient’s capacity for treatment must also be
consid-ered in the treatment plan. For example, a patient with schizo-phrenia
may agree to medication but be too disorganized to take it reliably without
help. Suitability for exploratory psychotherapy depends upon such factors as
the ability to observe oneself, toler-ate unpleasant affects, and establish and
maintain a working rela-tionship with the treater (Strupp and Binder, 1984).
Such factors must be evaluated in the interview.
Related Topics