Chapter: Essentials of Psychiatry: The Psychiatric Interview: Settings and Techniques
Database Components
Database Components
Identifying Data
This information establishes the patient’s identity, especially for the purpose of obtaining past history from other contacts, when necessary, as well as to fix his/her position in society. The pa-tient’s name should be recorded, along with any nickname or al-ternative names he/she may have been known by in the past. This is important for women who might have been treated previously under a maiden name, or a patient who has had legal entangle-ments and so has adopted aliases.
Date of birth, or at least age, and race are other
essen-tial parts of every person’s database. A number of different
classifications for race exist, as well as different terms and con-troversies
(Porter, 1993). In the USA and Canada, the categories of white, black (or
African-American), Asian, Native American, and others are generally accepted.
The additional modifier of ethnicity, especially Hispanic/nonHispanic, is
becoming more widely used. If a patient is a member of a particular subculture
based on ethnicity, country of origin, or religious affiliation, it may be
noted here.
A traditional part of the identifying data is a
reference to the patient’s civil status: single, married, separated, divorced,
or widowed. The evolution of relationship patterns over the last two decades,
with less frequent formalization of rela-tionships, has made classification
more difficult (Ishii-Kuntz and Tallman, 1991), especially in the case of
homosexual pa-tients, whose relationships are not legally recognized in most
jurisdictions.
The patient’s social security number (or other
national ID number) can be a very useful bit of data when seeking informa-tion
from other institutions.
In most cases, it is assumed that the informant
(supplier of the history) is the patient. If other sources are used, and
espe-cially if the patient is not the primary informant, this should be noted
at the beginning of the database.
Chief Complaint
The chief complaint is the patient’s responses to
the question, “What brings you to see me/to the hospital today?” or some
vari-ant. It is usually quoted verbatim, placed within quotation marks, and
should be no more than one or two sentences.
Even if the patient is very disorganized or
hostile, quoting his response can give an immediate sense of where the patient
is as the interview begins. If the patient responds with an exple-tive, or a
totally irrelevant remark, the reader of the database is immediately informed
about how the rest of the information may be distorted. In such cases, or if
the patient gives no response, a brief statement of how the patient came to be
evaluated should be made and enclosed in parentheses.
History of the Present Illness
Minimum Essential Database
The present illness history should begin with a
brief description of the major symptoms which brought the patient to
psychiatric attention. The most troubling symptoms should be detailed
ini-tially; later a more thorough review will be stated. As a minimum, the
approximate time since the patient was last at his baseline level of
functioning, and in what way he is different from that now, should be
described, and any known stressors, the sequence of symptom development, and
the beneficial or deleterious effects of interventions included.
How far back in a patient’s history to go,
especially when he has chronic psychiatric illness, is sometimes problematic.
In patients who have required repeated hospitalization, a summary of events
since last discharge (if within 6 months) or last stable baseline is indicated.
It is rare that more than 6 months of his-tory be included in the history of
the present illness, and detailed history is more commonly given on the past
month.
Expanded Database
A more expanded description of the history of the
present illness would include events in a patient’s life at the onset of
symptoms, as well as exactly how the symptoms have affected the patient’s
occupational functioning and important relationships. Any concurrent medical
illness symptoms, medication usage (and particularly changes), alterations in
the sleep–wake cycle, appe-tite disturbances and eating patterns should be
noted; significant negative findings should also be remarked upon.
Past Psychiatric History
Minimum Essential Database
Most of the major psychiatric illnesses are chronic
in nature. For this reason, often patients have had previous episodes of
illness with or without treatment. New onset of symptoms, without any previous
psychiatric history, becomes increasingly important with advancing age in terms
of diagnostic categories to be con-sidered. At a minimum, the presence or
absence of past psychi-atric symptomatology should be recorded, along with
psychiatric interventions taken and the result of such interventions. An
ex-plicit statement about past suicide and homicide attempts should be
included.
How far
back in a patient’s history to go, especially when he has chronic psychiatric
illness, is sometimes problematic. In patients who have required repeated
hospitalization, a summary of events since last discharge (if within 6 months)
or last stable baseline is indicated. It is rare that more than 6 months of
his-tory be included in the history of the present illness, and detailed
history is more commonly given on the past month.
Past Medical History
Minimum Essential Database
In any clinical assessment, it is important to know
how a patient’s general health status has been. In particular, any current
medical illness and treatment should be noted (Slaby and Andrew, 1987), along
with any major past illness requiring hospitalization. Pre-vious endocrine or
neurological illness are of particular perti-nence (Flomenbaum and Altman,
1985)
Expanded Database
An expanded database could well include significant
childhood illnesses, how these were handled by the patient and his fam-ily, and
therefore the degree to which the patient was able to develop a sense of
comfort and security about his physical well-being. Illnesses later in life
should be assessed for the degree of regression produced. The amount of time a
patient has had to take off work, how well he/she was able to follow a regimen
of medical care, his/her relationship with the family physician or treating
specialist can all be useful in predicting future re-sponse to treatment. A
careful past medical history can also at times bring to light a suicide
attempt, substance abuse, or dangerously careless behavior, which might not be
obtained any other way.
Family History
Minimum Essential Database
Given the evidence for familial, genetic factors in
so many psychiatric conditions, noting the presence of mental illness in
biological relatives of the patient is a necessary part of any database (Hammen
et al., 1987). It is important to
specify during questioning the degree of family to be considered – usually to
the second degree: aunts, uncles, cousins and grandparents, as well as parents,
siblings and children.
Expanded Database
A history of familial medical illness is a useful
part of an ex-panded database. A genogram (pedigree), including known fam-ily
members with dates and causes of death and other known chronic illnesses is
helpful. Questioning about causes of death will also occasionally bring out
hidden psychiatric illness, for example, sudden, unexpected deaths which were
likely suicides or illness secondary to substance abuse.
Personal History
Minimum Essential Database
Recording the story of a person’s life can be a
daunting under-taking and is often where a database can expand dramatically. As
a minimum, this part of the history should include where a patient was born and
raised, and in what circumstances – intact family, number of siblings and
degree of material comfort. Note how far the patient went in school, how he/she
did there, and what his/her occupational functioning has been. If he/she is not
working, why not? Has the patient ever been involved in crimi-nal activity, and
with what consequences? Has the patient ever married or been involved in a
committed relationship? Are there any children? What is his/her current source
of support? Does he/she live alone or with someone? Has he/she ever used
alcohol or other drugs to excess, and is there current use? Has he/she ever
been physically or sexually abused or been the victim of some other trauma?
Expanded Database
An expanded database can include a great deal of
material begin-ning even prior to the patient’s conception. What follows is an
outline of the kind of data which may be gathered, along with an organizational
framework.
Family of Origin
Were parents married or in committed relationships?
Personality and significant events in life of
mother, father, or other significant caregiver.
Siblings: how many? their ages, significant life
events, person-ality, relationship to patient.
Who else shared the household with the family?
Prenatal and Perinatal
Was the pregnancy planned? Quality of prenatal
care; mother’s and father’s response to pregnancy.
Illness, medication or substance abuse, smoking,
trauma dur-ing pregnancy; labor – induced or spontaneous?
Weeks gestation, difficulty of delivery, vaginal or
Caesarean section.
Presence of jaundice at birth, birth weight, Apgar
score.
Baby went home with mother or stayed on in
hospital.
Early
Childhood
Developmental milestones: smiling, sitting,
standing, walk-ing, talking, type of feeding – food allergies or intolerance.
Consistency of caregiving: interruptions by
illness, birth of siblings.
Reaction to weaning, toilet-training, maternal
separation. Earliest memories: problematic behavior (tantrums, bedwetting,
hair-pulling or nail-biting).
Temperament (shy, overactive, outgoing, fussy).
Sleep problems: insomnia, nightmares, enuresis,
parasomnias.
Later
Childhood
Early school experiences: evidence of separation
anxiety.
Behavioral problems at home or school: firesetting,
bedwetting, aggressive toward others, cruelty to animals, nightmares.
Developmental milestones: learning to read, write.
Relationships with other children and family: any
loss or trauma.
Reaction to illness.
Adolescence
School performance: ever in special classes?
Athletic abilities and participation in sports.
Evidence of gender identity concerns: overly
“feminine” or “masculine” in appearance/behavior, or perception by peers.
Ever run away? Able to be left alone and assume
responsibility. Age onset of puberty (menarche or nocturnal emissions),
reaction to puberty.
Identity
Sexual preference and gender identity, religious
affiliation (same as parents?).
Career goals: ethnic identification.
Sexual
History
Early sexual teaching: earliest sexual experiences,
experi-ence of being sexually abused, attitudes toward sexual behavior.
Dating history, precautions taken to prevent
sexually transmit-ted diseases and/or pregnancy.
Episodes of impotence and reaction.
Masturbating patterns and fantasies.
Preoccupation with particular sexual practices,
current sex-ual functioning, length of significant relationships, ages of
partners.
Age at which left home, level of educational
attainments. Employment history, relationships with supervisors and peers at
work, reasons for job change.
History of significant relationships including
duration, typical roles in relationships, patterns of conflict: mari-tal
history, legal entanglements and criminal history, both covert and detected,
ever victim or perpetrator of violence.
Major medical illness as adult.
Participation in community affairs.
Financial status: own or rent home, stability of
living situation. Ever on disability or public assistance?
Current family structure, reaction to losses of
missing mem-bers (parents, siblings), if applicable.
Substance abuse history.
Mental Status Examination
It can be helpful to conceptualize the recording of
the Men-tal Status Examination as a progression. One begins with a snapshot:
what can be gained from a cursory visual exam, without any movement or
interaction – appearance and affect. Next, motion is added: behavior. Then
comes sound: the pa-tient’s speech, though initially only as sound. The ideas
being expressed come next: the thought process and content, per-ception,
cognition, insight, and judgment. Table 3.5 gives a summary of areas to be
commented on, along with common terms.
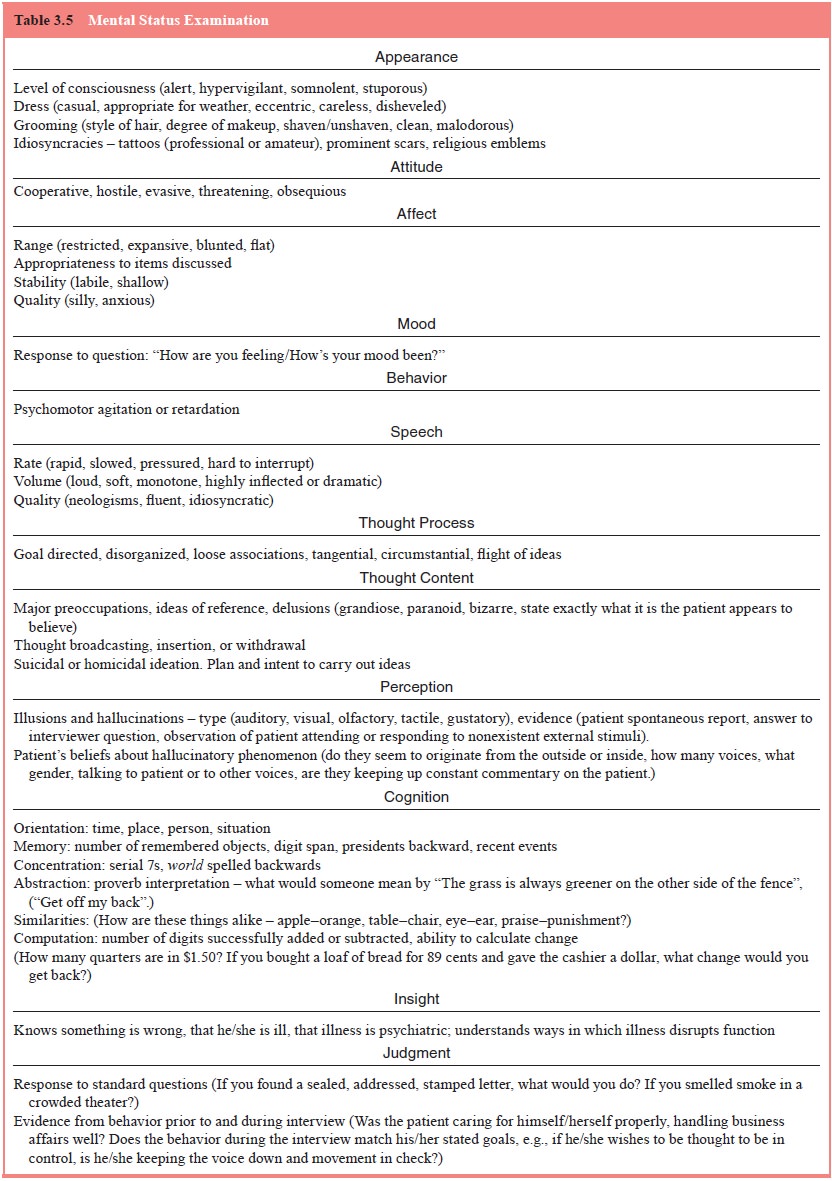
At every level of the Mental Status Examination,
prefer-ence should be given for explicit description over jargon. Stating that
a patient is delusional is less helpful than describing him as believing that
his neighbors are pumping poisonous gases into his bedroom while he sleeps.
Related Topics