Chapter: Essentials of Anatomy and Physiology: Urinary System and Fluid Balance
Urine Production
URINE PRODUCTION
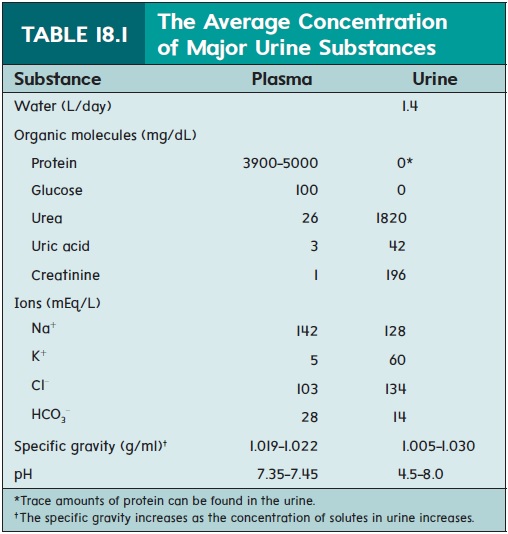
The primary function of the kidney is regulation of body fluid com-position. The kidney is the organ that sorts the substances from the blood for either removal in the urine or return to the blood. Substances that are waste products, toxins, and excess materials are permanently removed from the body, whereas other substances need to be con-served to maintain homeostasis. The structural components that per-form this sorting are the nephrons, the functional units of the kidney. If you have ever decided to organize your “junk” drawer in your desk or kitchen, you may realize just how difficult it is to quickly sort through all its contents. In fact, you may have found yourself simply emptying the drawer onto a table and then sorting the contents one by one as you place objects into a “save” group or a “throw away” group. In a sense, the kidney uses the same approach when regulating blood composition. The “throw away” items end up in the urine, and the “save” items go back into the blood. Urine is mostly water and some organic waste products, as well as excess ions (table 18.1).
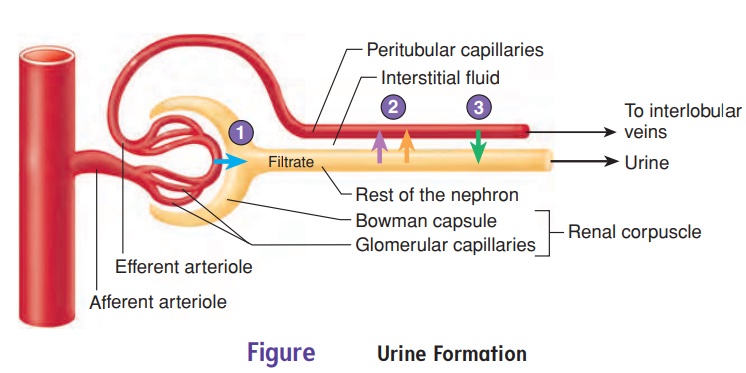
Scientists usually categorize urine formation into three major processes: filtration, tubular reabsorption, and tubular secretion (figure 18.7).
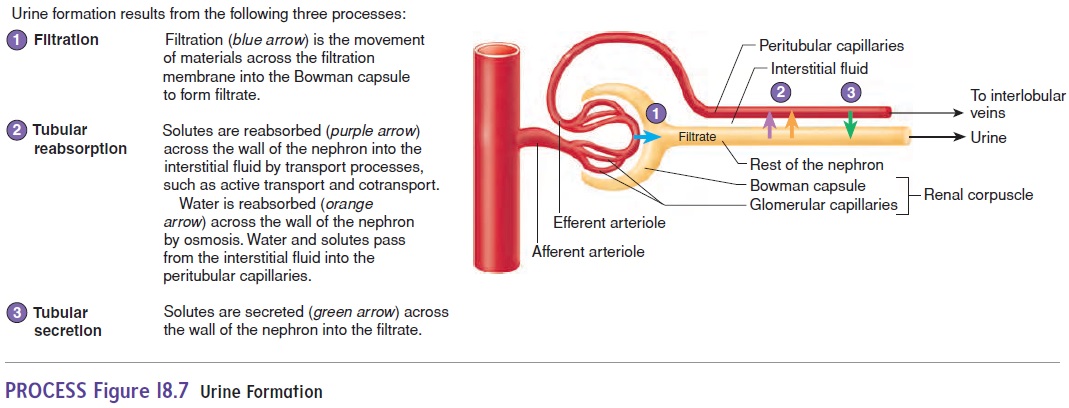
Filtration occurs when blood pressure nonselectively forceswater and other small molecules out of glomerular capillaries and into the Bowman capsule, forming a fluid called filtrate.
Tubular secretion is the active transport of solutes acrossthe nephron walls into the filtrate. Consequently, urine consists of substances that are filtered across the filtration membrane and those that are secreted from the peritubular capillaries into the nephron, minus the substances that are reabsorbed.
Filtration
An average of 21% of the blood pumped by the heart each minute flows through the kidneys. Of the total volume of blood plasma that flows through the glomerular capillaries, about 19% passes through the filtration membrane into the Bowman capsule to become fil-trate. In all the nephrons of both kidneys, about 180 liters (L) of filtrate are produced each day, but only about 1% or less of the filtrate becomes urine because most of the filtrate is reabsorbed.
Filtration is a nonspecific process whereby materials are sepa-rated based on size or charge. A simple example of size filtration is demonstrated by a drip coffeemaker. In this case, the driving force of filtration is gravity. The kidneys also use size filtration to remove substances from the blood by filtering it, but in this case, the driving force of this filtration is blood pressure.
The filtration membrane allows some substances, but not oth-ers, to pass from the blood into the Bowman capsule. Water and small solutes readily pass through the openings of the filtration membrane, but blood cells and most proteins, which are too large, do not enter the Bowman capsule. One example of a small blood protein that can enter the filtrate in very small amounts is albumin. Consequently, the filtrate contains no cells and little protein.
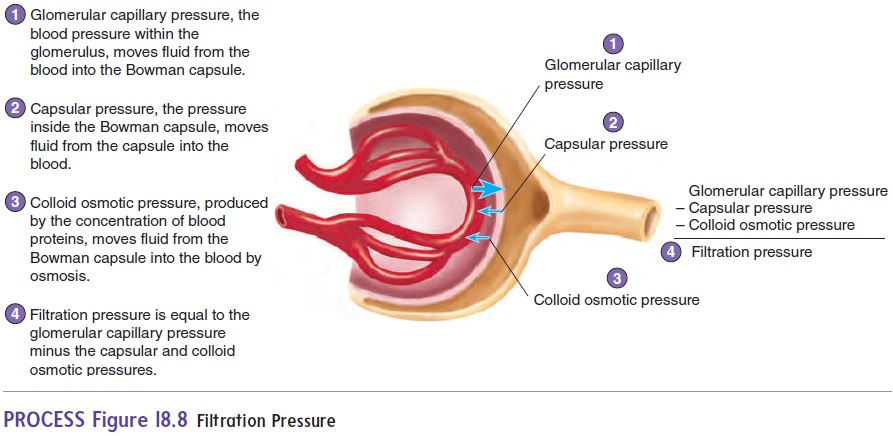
Glomerular capillary pressure
Capsular pressure
Colloid osmotic pressure
Filtration pressure
The filtration pressure forces fluid from the glomerulus into the Bowman capsule because the glomerular capillary pressure is greater than both the capsular and the colloid osmotic pressures. Under most conditions, the filtration pressure remains within a narrow range of values. However, when the filtration pressure increases, both the filtrate volume and the urine volume increase, and when the filtration pressure decreases, both the filtrate volume and the urine volume decrease.
The filtration pressure is influenced by the blood pressure in the glomerular capillaries, the blood protein concentration, and the pressure in the Bowman capsule. The blood pressure is normally higher in the glomerular capillaries than it is in most capillaries. The filtration pressure increases if the blood pressure in the glomerular capillaries increases further. The filtration pressure decreases if the blood pressure in the glomerular capillaries decreases.
The filtration pressure is also influenced by the concentration of proteins in the blood. An increase in blood protein concentration encourages the movement of water by osmosis back into the glomeru-lar capillaries and therefore reduces the overall filtration pressure . On the other hand, a decrease in blood protein con-centration inhibits the movement of water by osmosis back into the glomerular capillaries, which increases the overall filtration pressure.
Regulation of Filtration
The blood pressure within the glomerular capillaries is fairly con-stant because the afferent and efferent arterioles either dilate or con-strict to regulate the blood pressure there, even though the systemic blood pressure may fluctuate substantially. Also, the concentration of blood proteins and the pressure inside the Bowman capsule are fairly constant. As a consequence, the filtration pressure and the rate of filtrate formation are maintained within a narrow range of values most of the time.
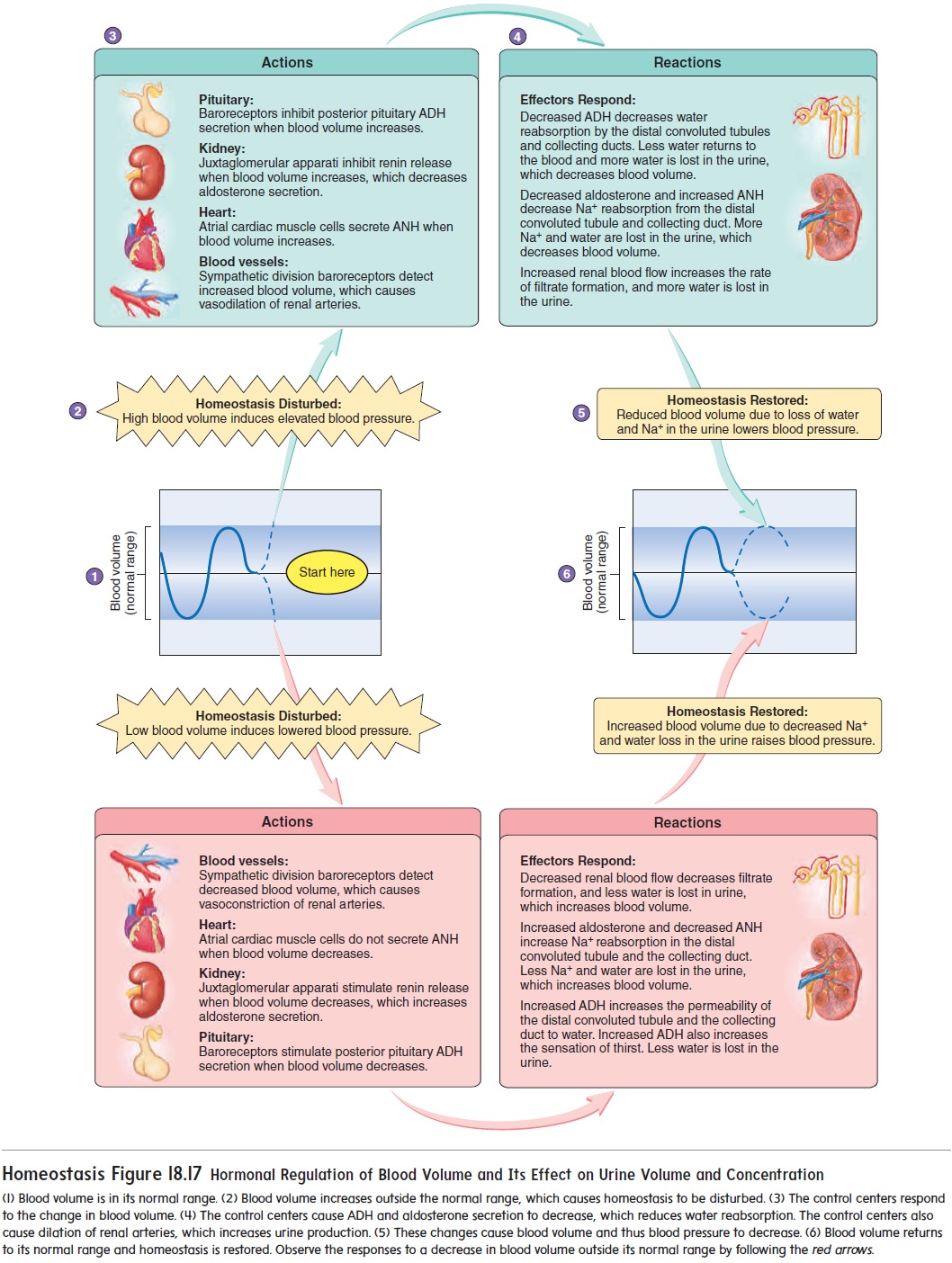
However, the filtration pressure does change dramatically under some conditions. Sympathetic neurons innervate the blood vessels of the kidney. Sympathetic stimulation constricts the arteries, causing a decrease in renal blood flow and filtrate formation in proportion to the intensity of the stimulation. It is possible to decrease filtrate forma-tion to only a few milliliters per minute. Consequently, only a small volume of urine is produced (see figure 18.17). For instance, during cardiovascular shock, the filtration pressure and filtrate formationfall dramatically. One of the dangers of cardiovascular shock is that the renal blood flow can be so low that the kidneys suffer from lack of O2. If the O2 level remains too low for a long enough time, permanent kidney damage or complete kidney failure results. One important reason for treating cardiovascular shock quickly is to avoid damage to the kidneys. Other conditions, such as intense physical activity or trauma, also increase sympathetic stimulation of renal arteries and decrease urine production to very low levels. On the other hand, increased blood pressure decreases sympathetic stimulation of renal blood arteries, and urine volume increases (see figure 18.17).
In addition to the effects of blood pressure on filtration pres-sure, decreases in the concentration of plasma proteins, caused by conditions such as inflammation of the liver, where most of the blood proteins are produced, increase the filtration pressure. The increased filtration pressure causes the filtrate and urine volume to increase.
Tubular Reabsorption
As the filtrate flows from the Bowman capsule through the proxi-mal convoluted tubule, loop of Henle, distal convoluted tubule, and collecting duct, many of the solutes in the filtrate are reabsorbed. About 99% of the original filtrate volume is reabsorbed and enters the peritubular capillaries. The reabsorbed filtrate flows through the renal veins to enter the general circulation. Only 1% of the orig-inal filtrate volume becomes urine (figure 18.9). Because excess ions and metabolic waste products are not readily reabsorbed, the small volume of urine produced contains a high concentration of ions and metabolic waste products.
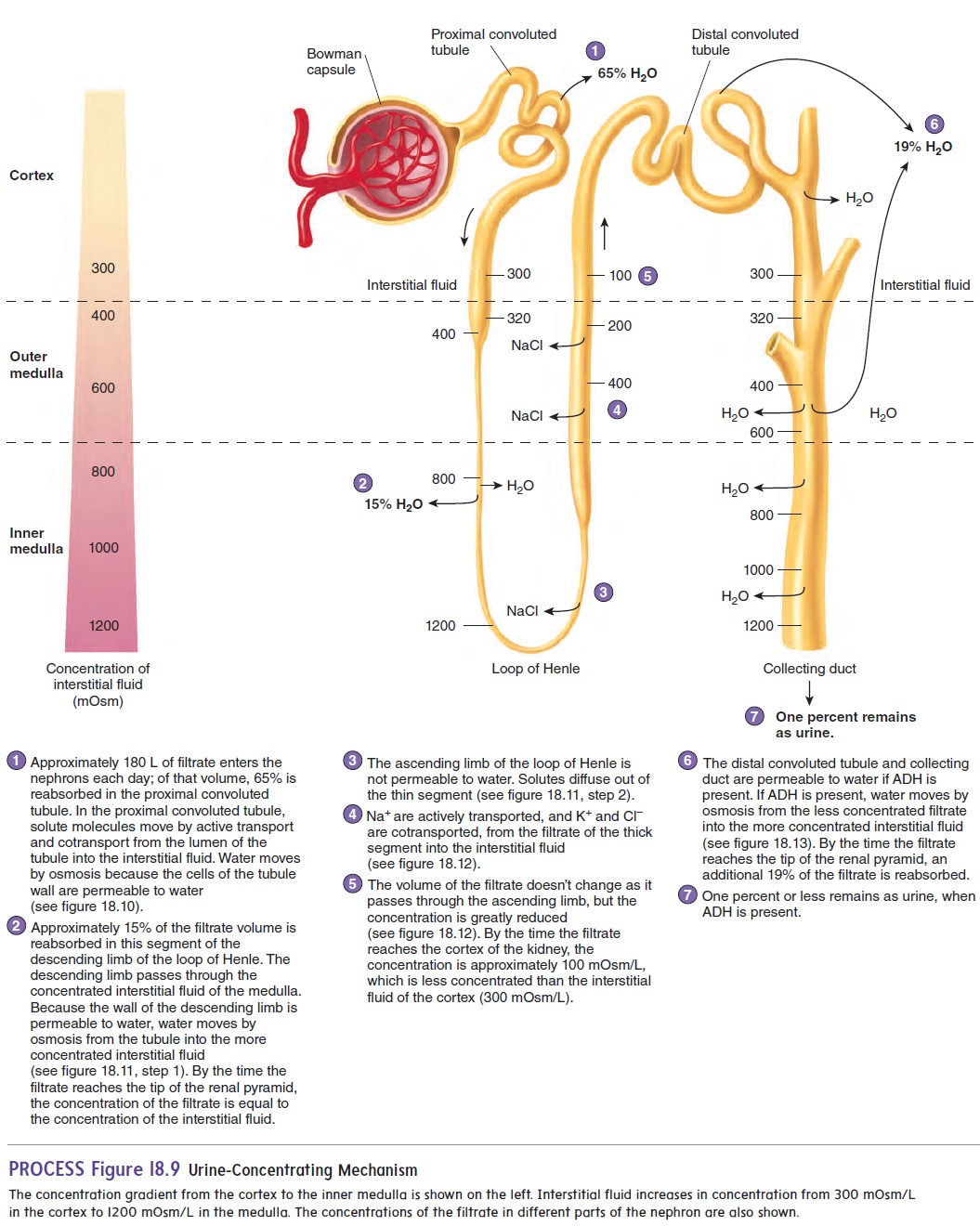
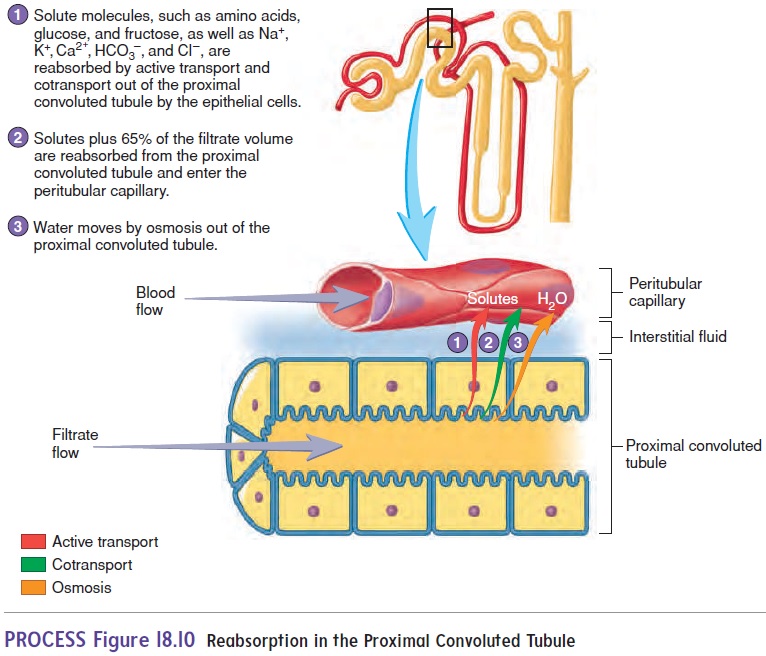
The proximal convoluted tubule is the primary site for the reabsorption of solutes and water. The cuboidal cells of the proximal convoluted tubule have numerous microvilli and mito-chondria, and they are well adapted to transport molecules and ions across the nephron wall by active transport and cotransport. Substances transported from the proximal convoluted tubule include proteins, amino acids, glucose, and fructose molecules, as well as Na+, K+, Ca2+, HCO3−, and Cl−. The proximal convoluted tubule is permeable to water. As solute molecules are transported out of the proximal convoluted tubule into the interstitial fluid, water moves by osmosis in the same direction. The solutes and water then enter the peritubular capillaries. Consequently, 65% of the filtrate volume is reabsorbed from the proximal convoluted tubule (figures 18.9, step 1, and 18.10).
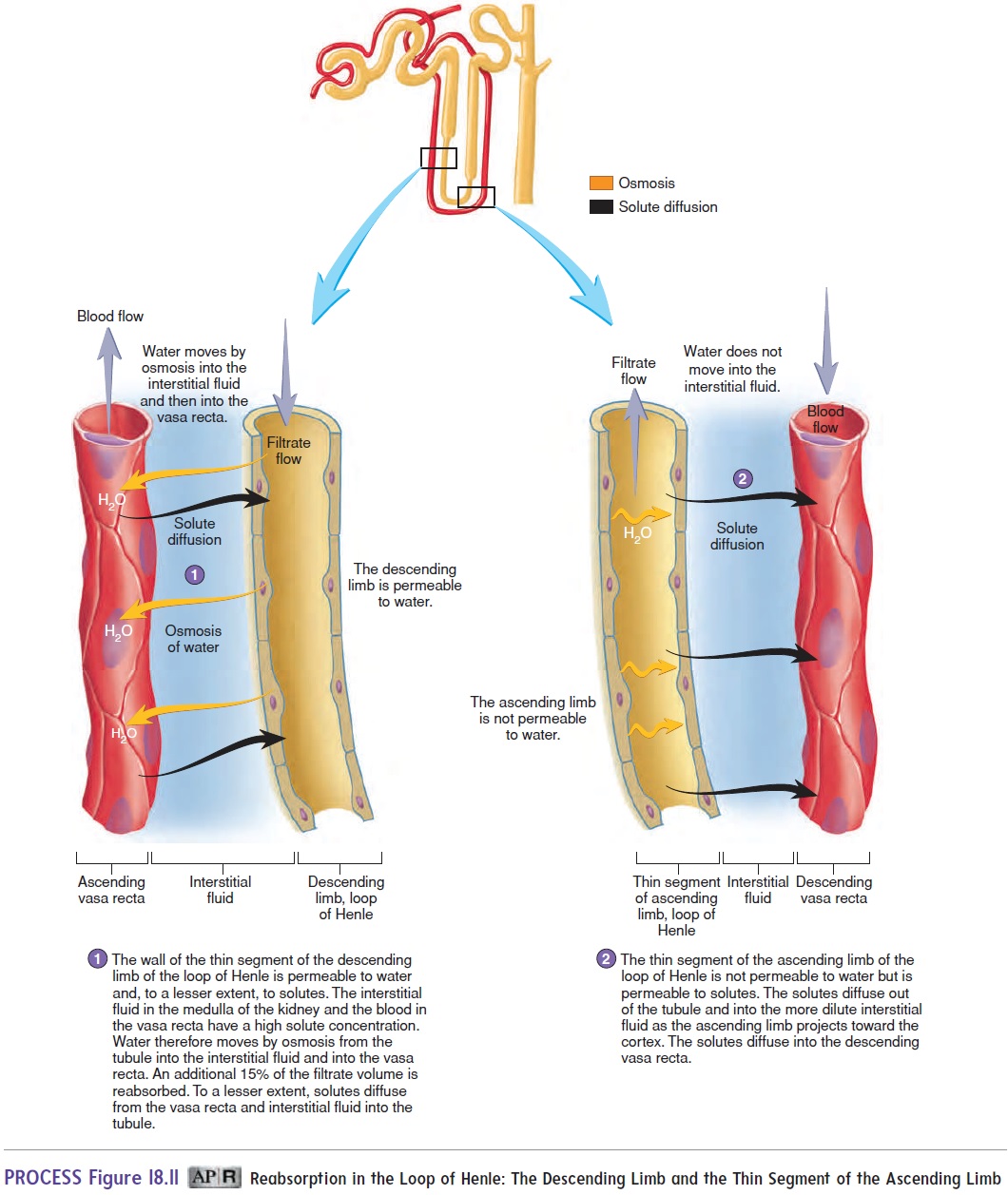
The descending limb of the loop of Henle further concentrates the filtrate. The renal medulla contains very concentrated intersti-tial fluid that has large amounts of Na+, Cl−, and urea. The wall of the thin segment of the descending limb is permeable to water and moderately permeable to solutes. As the filtrate passes through the descending limb of the loop of Henle into the medulla of the kid-ney, water moves out of the nephron by osmosis, and some solutes move into the nephron by diffusion. By the time the filtrate has passed through the descending limb, another 15% of the filtratevolume has been reabsorbed, and the filtrate is as concentrated as the interstitial fluid of the medulla. The reabsorbed water and solutes enter the vasa recta (figure 18.11; see figure 18.9, step 2).
The ascending limb of the loop of Henle dilutes the filtrate by removing solutes. The thin segment of the ascending limb is not permeable to water, but it is permeable to solutes. Consequently, solutes diffuse out of the nephron (figure 18.11; see figure 18.9, step 3).
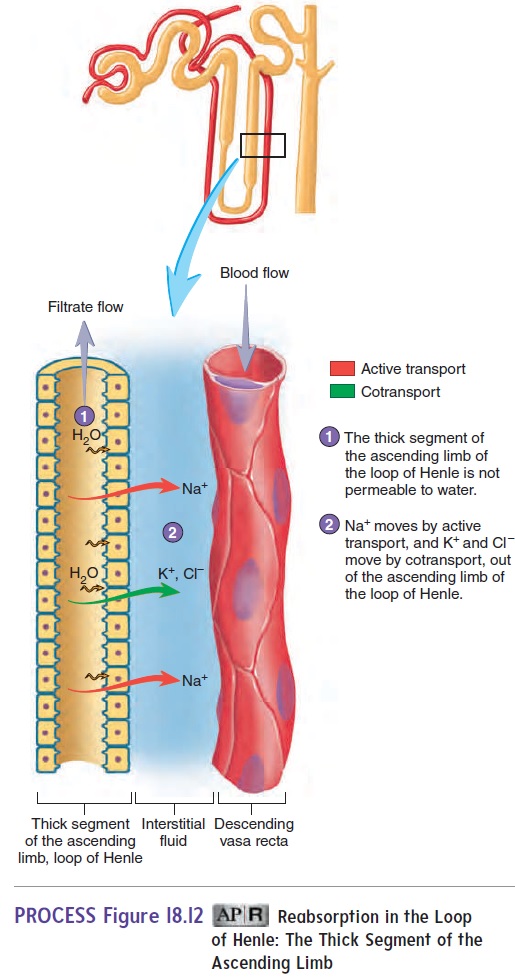
The cuboidal epithelial cells of the thick segment of the ascending limb actively transport Na+ out of the nephron, and K+ and Cl− are cotransported with Na+. The thick segment of the ascending limb is not permeable to water. As a result, Na+, K +, and Cl−, but little water, are removed from the filtrate (see figure 18.9, step 4). Because of the efficient removal of these solutes, the high-ly concentrated filtrate that enters the ascending limb of the loop of Henle is converted to a dilute solution by the time it reaches the distal convoluted tubule (figure 18.12; see figure 18.9, step 5). As the filtrate enters the distal convoluted tubule, it is more dilute than the interstitial fluid of the renal cortex. Also, because of the volume of filtrate reabsorbed in the proximal convoluted tubule and the descending limb of the loop of Henle, only about 20% of the original filtrate volume remains. The solutes transported from the ascending limb of the loop of Henle enter the interstitial fluid of the medulla and help keep the concentration of solutes in the medulla high. Excess solutes enter the vasa recta.
The cuboidal cells of the distal convoluted tubule and col-lecting duct remove water and additional solutes. Na+ and Cl− are reabsorbed. Sodium ions are actively transported, and chloride ions are cotransported. Also, 19% of the original filtrate volume is reabsorbed by osmosis, leaving about 1% of the original filtrate as urine (figure 18.13; see figure 18.9, steps 6 and 7). The reabsorbed water and solutes from the distal convoluted tubule enter the peri-tubular capillaries and the vasa recta from the collecting ducts.
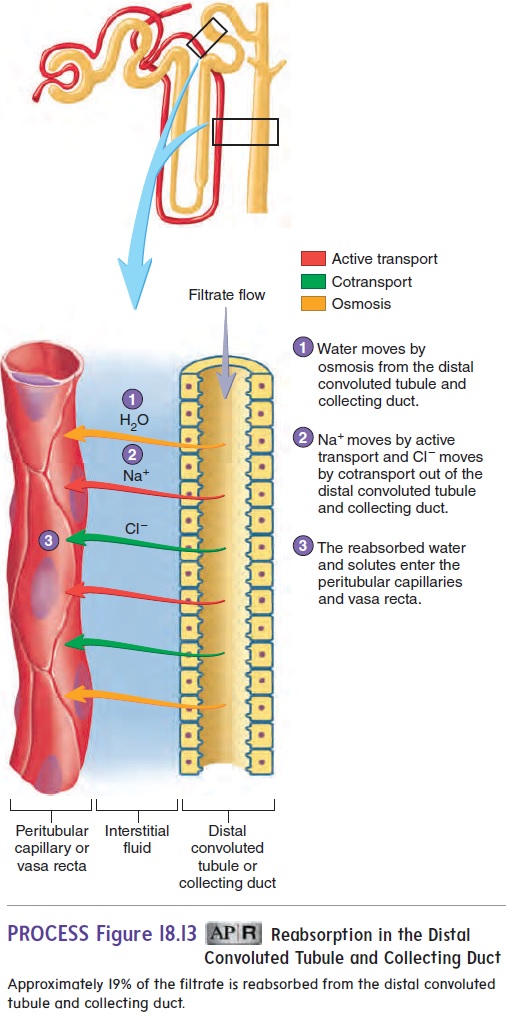
The reabsorption of water and solutes from the distal convo-luted tubule and collecting duct is controlled by hormones, which have a great influence on urine concentration and volume (see “Regulation of Urine Concentration and Volume”).
In summary, most of the useful solutes that pass through the filtration membrane into the Bowman capsule are reabsorbed in the proximal convoluted tubule. Filtrate volume is reduced by 65% in the proximal convoluted tubule and by 15% in the descending limb of the loop of Henle. In the ascending limb of the loop of Henle, Na+, K+, and Cl−, but little water, are removed from the filtrate. Consequently, the filtrate becomes dilute. In the distal convoluted tubule and the collecting duct, additional Na+ and Cl− are removed, water moves out by osmosis, and the filtrate volume is reduced by another 19%, leaving 1% of the original filtrate volume as urine.
Tubular Secretion
Some substances, including by-products of metabolism that become toxic in high concentrations and drugs or other molecules not nor-mally produced by the body, are secreted into the nephron from the peritubular capillaries. As with tubular reabsorption, tubular secretion can be either active or passive. For example, ammonia diffuses into the lumen of the nephron, whereas H+, K+, creatinine, histamine, and penicillin are actively transported into the nephron.
Hydrogen ions are actively transported into the proximal con-voluted tubule. The epithelial cells actively transport large quanti-ties of H+ across the nephron wall into the filtrate. The secretion of H+ plays an important role in regulating the body fluid pH.
In the proximal convoluted tubule, K+ is reabsorbed. However, in the distal convoluted tubule and collecting duct, K+ is secreted, resulting in a net loss of K+ in the urine.
Related Topics