Chapter: Essentials of Anatomy and Physiology: Urinary System and Fluid Balance
Regulation of Extracellular Fluid Composition
REGULATION OF EXTRACELLULAR FLUID COMPOSITION
Homeostasis requires that the intake of substances equals their elimination. Needed water and ions enter the body by ingestion; excess water and ions exit the body by excretion. The amounts of water and ions entering and leaving the body can vary over the short term. For example, greater quantities of water and ions are lost in the form of perspiration on warm days than on cool days, and varying amounts of water and ions may be lost in the form of feces. However, over a long period, the total amount of water and ions in the body does not change unless the individual is grow-ing, gaining weight, or losing weight. Regulating the amounts of water and ions in the body involves the coordinated participation of several organ systems, but the kidneys are the most important, with the skin, liver, and digestive tract playing supporting roles. Two mechanisms help regulate the levels of ions in the extracel-lular fluid: thirst regulation and ion concentration regulation.
Thirst Regulation
Water intake is controlled by neurons in the hypothalamus, collec-tively called the thirst center. When blood becomes more concen-trated, the thirst center responds by initiating the sensation of thirst (figure 18.20). When water or another dilute solution is consumed, the blood becomes less concentrated and the sensation of thirst decreases. Similarly, when blood pressure drops, as occurs dur-ing shock, the thirst center is activated, and the sensation of thirst
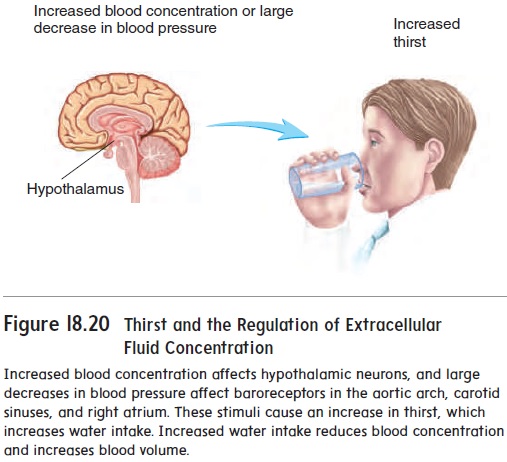
Figure 18.20 Thirst and the Regulation of extracellularFluid Concentration
is triggered. Consumption of water increases the blood volume and allows the blood pressure to return to its normal value. Other stimuli can also trigger the sensation of thirst. For example, if the mucosa of the mouth becomes dry, the thirst center is activated. Thirst is one of the important means of regulating extracellular fluid volume and concentration.
Ion Concentration Regulation
If the water content or concentration of ions in the extracellular fluid deviates from its normal range, cells cannot control the move-ment of substances across their cell membranes or the composition of their intracellular fluid. The consequence is abnormal cell func-tion or even cell death. Keeping the extracellular fluid composition within a normal range is therefore required to sustain life.
Regulating the concentrations of positively charged ions, such as Na+, K+, and Ca2+, in the body fluids is particularly important. Action potentials, muscle contraction, and normal cell membrane permeability depend on the maintenance of a narrow range of concentrations for these ions. Important mechanisms control the concentrations of these ions in the body. Negatively charged ions, such as Cl−, are secondarily regulated by the mechanisms that con-trol the positively charged ions. The negatively charged ions are attracted to the positively charged ions; when the positively charged ions are transported, the negatively charged ions move with them.
Sodium Ions
Sodium ions (Na+) are the dominant ions in the extracellular fluid.About 90–95% of the osmotic pressure of the extracellular fluid results from sodium ions and from the negative ions associated with them.
The recommended intake of Na+ is 2.4 grams per day (g/day), because of its association with high blood pressure in some people. Most people in the United States consume two to three times the recommended amount of Na+. The kidneys provide the major route by which the excess Na+ is excreted.
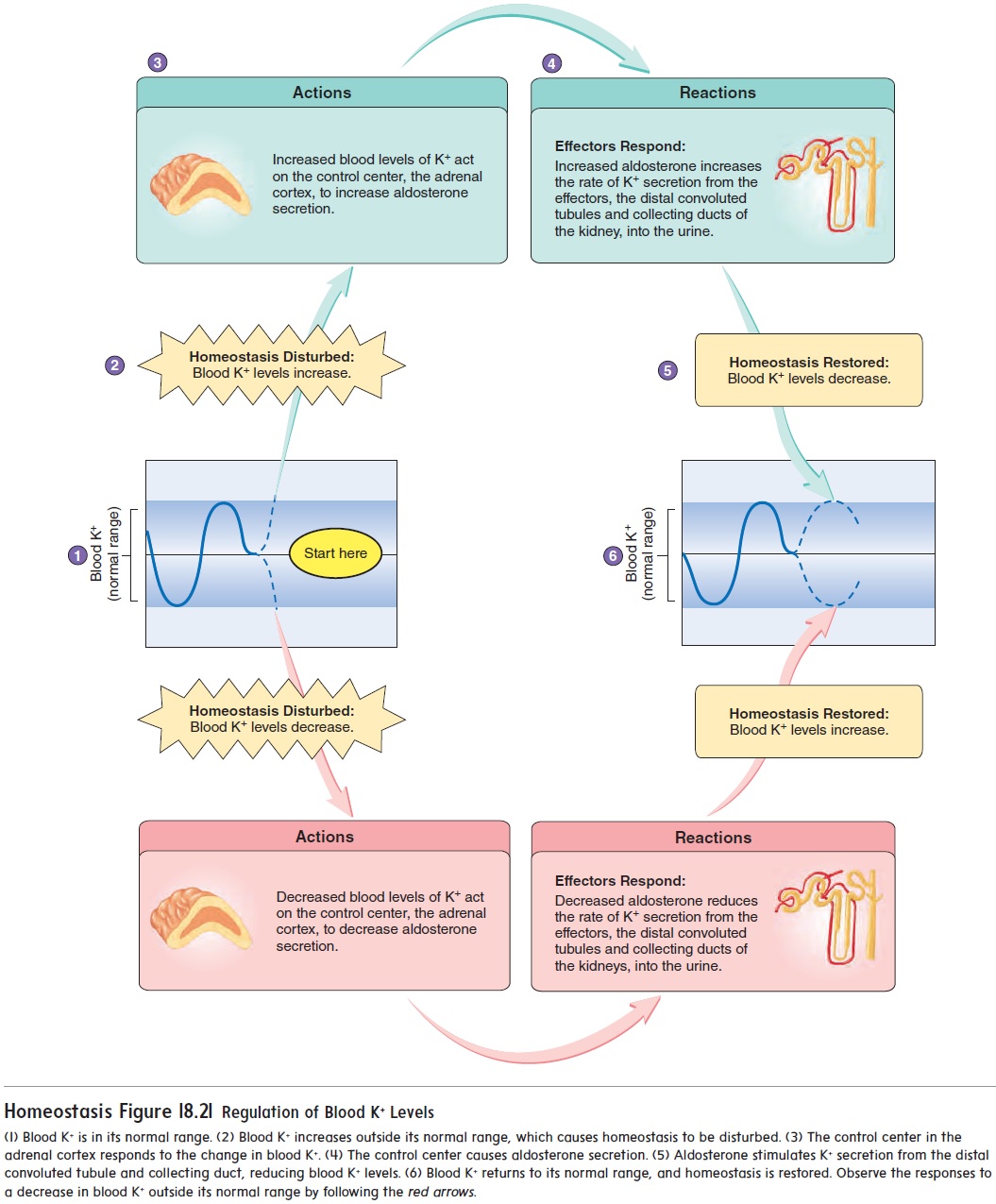
Stimuli that control aldosterone secretion influence the reabsorp-tion of Na+ from nephrons of the kidneys and the total amount of Na+ in the body fluids. Reabsorption of Na+ from the distal convoluted tubules and collecting ducts is very efficient, and little Na+ is lost in the urine when aldosterone is present. When aldosterone is absent, reabsorption of Na+ in the nephron is greatly reduced, and the amount of Na+ lost in the urine increases. Aldosterone also plays an essential role in regulating the extracellular K+ concentration (figure 18.21).
Sodium ions are also excreted from the body in perspiration, or sweat. Normally, only a small quantity of Na+is lost each day in theform of sweat, but the amount increases during heavy exercise in a warm environment.
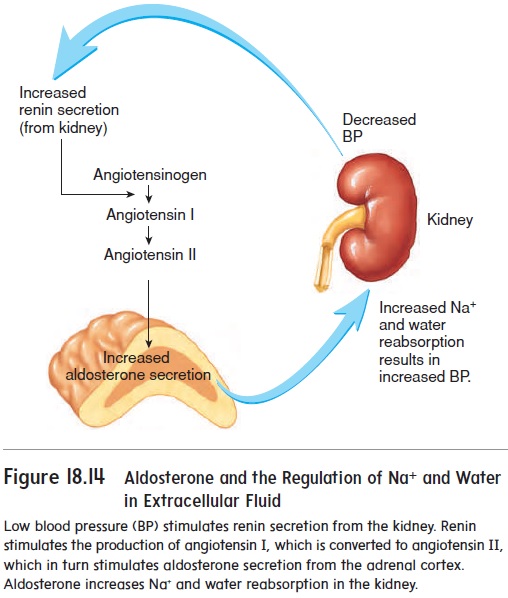
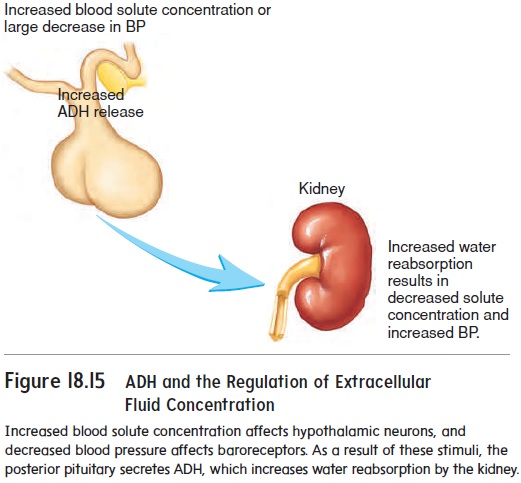
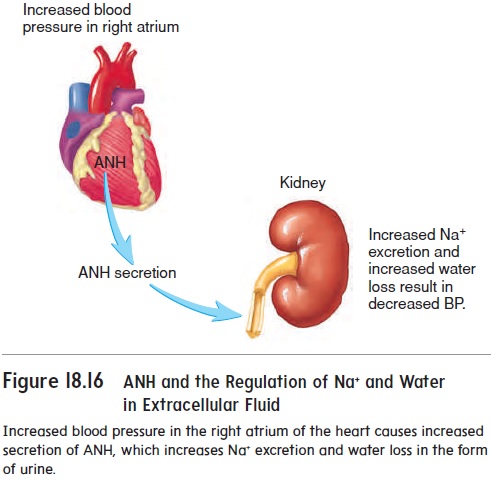
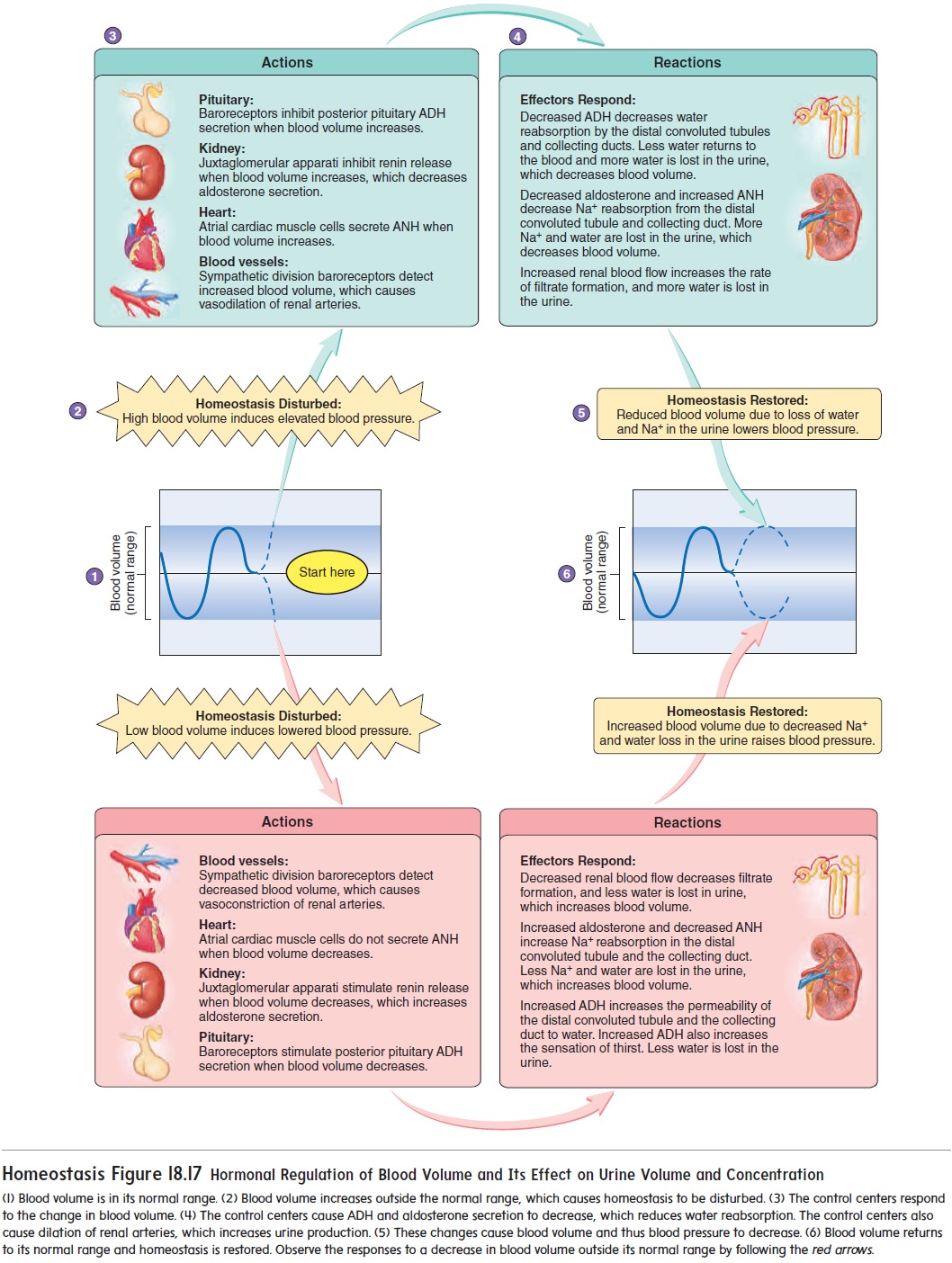
Because Na+ has such a large effect on the osmotic pressure of the extracellular fluid, mechanisms that influence Na+ concentra-tions in the extracellular fluid also influence the extracellular fluid volume. The mechanisms that play important roles in controlling these levels are the renin-angiotensin-aldosterone mechanism, the atrial natriuretic (ANH) mechanism, and antidiuretic hormone (ADH) (see figures 18.14, 18.15, 18.16, and 18.17). For example, low blood pressure increases renin and ADH secretion. The result is an increase in Na+ and water reabsorption in the kidney to bring blood pressure and the Na+concentration back to their normal ranges. Increased blood pressure inhibits renin and ADH secretion, and stimulates ANH secretion. The result is a decrease in Na+ reab-sorption and an increase in urine production to bring blood pres-sure and the blood’s Na+ concentration into their normal ranges.
Potassium Ions
Electrically excitable tissues, such as muscles and nerves, are highly sensitive to slight changes in the extracellular K+ concentration. The extracellular concentration of K+ must be maintained within a narrow range for these tissues to function normally.
Aldosterone plays a major role in regulating the concentration of K+ in the extracellular fluid. Dehydration, circulatory system shock resulting from plasma loss, and tissue damage due to injuries such as severe burns all cause extracellular K+ concentrations to increase above normal. In response, aldosterone secretion from the adrenal cortex increases and causes K+ secretion to increase (figure 18.21).
If the K+ concentration in the extracellular fluid decreases, aldo-sterone secretion from the adrenal cortex decreases. In response, the rate of K+ secretion by the kidneys is reduced (figure 18.21).
Calcium Ions
The extracellular concentration of Ca2+, like that of other ions, is maintained within a narrow range. Increases and decreases in the extracellular concentration of Ca2+ have dramatic effects on the elec-trical properties of excitable tissues. For example, decreased extra-cellular Ca2+ concentrations make cell membranes more permeable to Na+, thus making them more electrically excitable. Decreased extracellular concentrations of Ca2+ cause spontaneous action poten-tials in nerve and muscle cells, resulting in hyperexcitability and muscle tetany. Increased extracellular Ca2+ concentrations make cell membranes less permeable to Na+, thus making them less electrical-ly excitable. Increased extracellular concentrations of Ca2+ inhibit action potentials in nerve and muscle cells, resulting in reduced excitability and either muscle weakness or paralysis.
Parathyroid hormone (PTH), secreted by the parathyroidglands, increases extracellular Ca2+ concentrations. The rate of PTH secretion is regulated by the extracellular Ca2+ concentration (see figure 10.17). An elevated Ca2+ concentration inhibits the secretion of PTH and a reduced Ca2+ concentration stimulates the secretion of PTH. PTH causes osteoclasts to degrade bone and release Ca2+ into the body fluids. PTH also increases the rate of Ca2+ reabsorption from kidney nephrons.
Vitamin D increases Ca2+ concentration in the blood by increasing the rate of Ca2+ absorption by the intestine. Some vitamin D is consumed in food, and the body produces the rest . PTH affects the intestinal uptake of Ca2+ because PTH increases the rate of vitamin D production in the body.
Calcitonin (kal-si-tō′ nin) is secreted by the thyroid gland.Calcitonin reduces the blood Ca2+ concentration when it is too high. An elevated blood Ca2+ concentration causes the thyroid gland to secrete calcitonin, and a low blood Ca2+ concentration inhibits calci-tonin secretion. Calcitonin reduces the rate at which bone is broken down and decreases the release of Ca2+ from bone (see figure 10.17).
Phosphate and Sulfate Ions
Some ions, such as phosphate ions (PO43−) and sulfate ions(SO42−), are reabsorbed by active transport in the kidneys. Therate of reabsorption is slow, so that if the concentration of these ions in the filtrate exceeds the nephron’s ability to reabsorb them, the excess is excreted into the urine. As long as the concentration of these ions is low, nearly all of them are reabsorbed by active transport. This mechanism plays a major role in regulating the concentration of PO43− and SO42− in the body fluids.
Related Topics