Chapter: Forensic Medicine: Toxicology and alcohol
Toxicology in general
Toxicology in general
Classification
Toxicological substances (including medicines)
can be classified according to the following:
·
chemical characteristics, for example organic, inorganic
·
mode of action, for example corrosive, irritant
·
target organ, for example lungs, heart
·
intended use, for example solvent, insecticide
·
field of use, for example agricultural, industrial
·
origin, for example plant, bacterial, fungal
Factors affecting toxicity
A poison is a substance which, when absorbed by
a living organism, results in harm or death. There are many thousands of
substances occurring naturally or in synthesised form that exhibits this
property. Medicines or even beverages, if used in excess or inappropriately,
can result in poisoning. Furthermore, two innocuous substances could, after
administration, combine and so have a harmful synergistic effect.
Poisoning can be acute, subacute or chronic and
its intensity as well as its signs and symptoms can vary from person to person,
appearing dramatically and suddenly or as vague discomfort over a long time. It
may also vary in the same individual at different times.
The intensity and nature of the reaction to a poison often becomes an important issue in court. The many variables which need to be considered when attempting to solve this problem are best expressed as a functional equation:
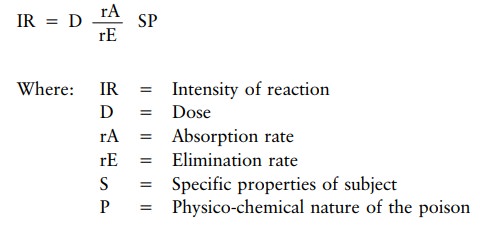
Intensity of the reaction ranges from the most insignificant to death.
Dose is
the amount administered and the frequency of administration.
Rate of absorption will be influenced by the route of administration, that is whether by
mouth, intravenously, per vagina, per rectum, or by inunction (rubbing in) or
inhalation.
Rate of elimination may be accelerated by vomiting, diarrhoea or accelerated metabolic
pathways such as in people addicted to the particular substance or habitually
exposed to it in the workplace. Both absorption and elimination may be delayed
by a variety of medicines in use at the relevant time. The converse is equally
true.
The specific properties of the subject include hypersensitivity, various diseases, as
well as the inherent biological variability of living material even in the same
population group, and expressed graphically as an S-shaped curve when dose is
plotted against percentage response in the group at each varying dose level.
The physico-chemical nature of the poison (solid, gaseous, liquid, soluble) is also an
important variable in the equation.
The difference between a therapeutic and a lethal dosage
As already stated in the explication of the
formula, the response to a given dose is not always the same in all
individuals. Some individuals may show the same reaction at a lower dose than
another individual will show at a significantly higher dose. This is due to
specific features, which not only differ from individual to individual, but can
also differ in the same individual from day to day. In other words, there are
interpersonal as well as intrapersonal differences in the reaction to a given
dose. This reaction can be represented graphically by a sigmoid or S-shape (fig
11.1).
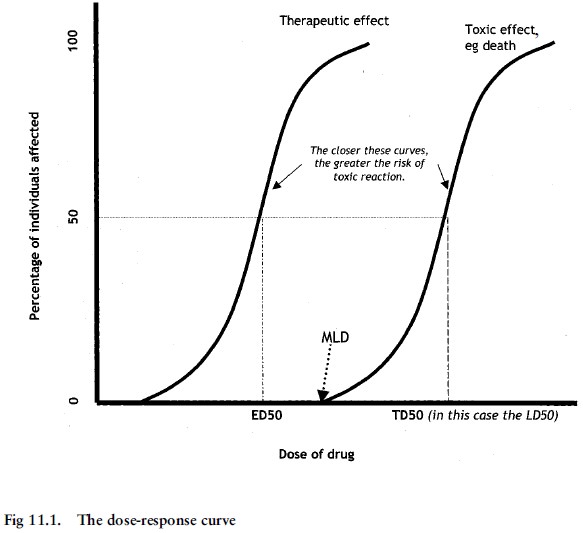
The therapeutic dose where 50% of individuals
will experience the therapeutic effect is also known as the ED50 (``effective
dose''). The dose where 50% of indiduals will die, is called LD50 (``lethal
dose''). If a specific toxic effect other than death is used, it is called TD50
(``toxic dose''). The closer these doses are to one another, the higher the
risk for toxic reactions. The concept of the minimum lethal dose or MLD has
been debated at length. It is obvious from the sigmoid curve that we could say
that the drug could not have caused the individual's death if the level is
lower than the MLD. The contrary, however, is not possible; if an individual's
blood level is somewhere along this curve, it is not possible to state whether
the individual indeed died due to the effect of the drugs or substance. The
higher the level of the substance, the greater the chances that it could have
played a role.
Poisoning
How is poisoning proved?
Poisoning can be proved from the symptoms and
signs displayed by the victim during his lifetime, together with a chemical
analysis to test for the presence of a particular poison or its metabolites in
the vomit, bodily excretions, and blood, or by determining specific
target-organ changes. At a post-mortem examination internal organs and tissues
can be removed from the body for chemical analysis.
If the poison is taken by mouth, it must (after
absorption from the gut) pass to the liver. The liver can destroy the poison or
modify it, or the poison can damage the liver. This can lead to symptoms and
signs indicating liver disorder, but often there is no clinical evidence to indicate
whether the damage is due to disease or poisoning. There could for example, be
jaundice (a yellow colouring of the skin, internal organs and tissues) because
the ability of the liver to handle the bile pigments could be sufficiently
disrupted to push the bile back into the blood. This is one of the ways in
which jaundice can originate regardless whether by disease or by a poison. One
can now understand why the liver is often one of the organs sent for chemical
analysis in a case of suspected poisoning.
After passing through the liver the poison
reaches the heart and then goes to the brain and all the other organs and
tissues of the body. It is eventually eliminated in the sweat, urine and the
faeces. This is why the kidneys (which produce the urine) are also often sent
for analysis in the case of a deceased, or the urine in the case of a living
person.
The stomach and its contents can also be removed
at a post-mortem examination for analysis or, in the living patient, vomit can
be examined. Inspection of stomach contents can reveal recognisable items, for
example portions of the swallowed capsules which contained medicines, fragments
of the coloured wing cases of the beetles responsible for cantharadin (Spanish
fly) poisoning, et cetera. Some poisons have a greater affinity for certain
tissues. For example, arsenic is deposited in the hair and the nails, and hair
and nail clippings thus could provide evidence not only of this form of
poisoning, but also of the approximate period of time during which the arsenic
was ingested, because the tempo at which hair and nails grow is known. So, if
these specimens are analysed in sections along the length of the hair (or
nails), the likely time of ingestion of the poison can be determined.
In 1955 a lock of Napoleon's hair was shown to
contain arsenic. It was hinted that this might purposely have been administered
by his captors during the latter part of his life on St Helena. He experienced
health problems after the Russian debacle, and evidence suggests that since arsenic
was commonly prescribed as a tonic at the time, this probably was the source of
the arsenic.
If heavy metal poisons are found in tissues they
should be evaluated carefully, and the possibility that they may represent
environmental contamination before and after death must be carefully
considered. In certain parts of South Africa the soil is heavily contaminated
by arsenic, and the presence of arsenic in the hair or nails of exhumed bodies
may mean no more than post-mortem contamination of these tissues.
Post-mortem examinations seldom reveal any
characteristic signs which can be attributed to a particular poison. One of the
few notable exceptions is the bright, cherry-red colour of the blood in
carbon-monoxide poisoning, due to the formation of a special blood pigment
called carboxyhaemoglobin (COHb). Another example is the staining and
destruction of the skin around the lips and of the lining of the mouth, the
gullet and the stomach, produced by corrosive acids or caustic alkalis.
It is sometimes claimed that acute arsenic
poisoning produces characteristic haemorrhages beneath the inner lining of the
left ventricle of the heart. However, this is also seen in cases of death due
to other causes. Therefore, although such haemorrhages are not peculiar to arsenic
poisoning only, they may well arouse the suspicion of arsenic poisoning (in the
absence of any other satisfactory explanation for its appearance in the heart - see photo 49).
Lead and mercury poisoning can cause a dark
blue-black line along the gum-tooth margin, and in organophosphate poisoning
the lungs may appear markedly oedematous and frothy fluid may exude from the
mouth and nostrils (photo 47). Potassium dichromate can stain the tissues an
orange colour. It has also been observed that flies which feed from the body of
a person who died from insecticide poisoning also die. If there is a smell of
bitter almonds when the skull is opened, one should suspect cyanide poisoning.
Microscopic examination of the tissues could also indicate poisoning. Certain
changes in liver cells could indicate paracetamol poisoning, and in kidney
cells, glycol poisoning.
Remnants of capsule coverings, insects, and
leaves in the stomach contents could suggest the analytical procedure to be
followed during toxicological examination.
In general the post-mortem examination provides
little evidence to indicate a particular form of poisoning. The various organs
and systems affected by a poison however do display specific signs and
symptoms. Whatever the poison affecting the intestinal tract, the clinical
features are usually nausea, retching, vomiting, diarrhoea, constipation and
cramp (colic). In the same way, the effects of any poison acting on the
respiratory system are manifested in interference with the breathing, for example
the victim has difficulty in breathing in or breathing out; he breathes rapidly
or slowly; the breathing is deep or shallow; there may be a cough, et cetera.
Arsenic acts on almost every system of the body.
Hence, in chronic arsenic poisoning, where arsenic has been ingested over a
period of many weeks or months, the victim may show evidence of vomiting and
diarrhoea, thickening of the skin, especially of the palms and the soles,
uniform or spotty pigmentation of the skin, rashes of one kind or another,
inflammation of nerves in different parts of the body, producing, for example,
hoarseness of the voice or weakness of the limbs, sometimes amounting to
paralysis.
Arsenic poisoning has so many different faces
that it can be mistaken for many diseases. It could simulate laryngitis,
scarlet fever (because of the type of rash it produces), alcoholic neuritis,
and attacks of diarrhoea and vomiting, which could be (and often have been)
mistaken for bacterial food poisoning. The pigmentation of the skin could resemble
certain natural diseases associated with weakness of the limbs, vomiting, et
cetera.
The problem is, therefore, to decide whether the
different clinical signs as a group could have been caused by a natural disease
or by a poison. Otherwise one has to decide how much each contributes to the
total picture. The post-mortem examination thus becomes important in excluding
certain diseases, and the chemical analysis can provide confirmation of the
nature and amount of the poison, which will indicate what condition the victim
suffered from and what caused his death.
It is often the virtually negative findings at a
post-mortem examination which arouse suspicion about poison as a possible
explanation of the cause of death. A negative post-mortem finding thus becomes
a very important factor in the investigation of a case of suspected poisoning.
The clinical history, the post-mortem findings
and the results of any special investigations (such as the chemical analysis
for the presence of a poison) must all be evaluated in order to arrive at a
conclusion. The answer is not to be found in one isolated part of the inquiry,
but in a combination of all the steps involved in making a medical diagnosis.
Since the final cause of death in a case of
poisoning is often a condition such as pneumonia, liver failure or kidney
disease, it is understandable why, even despite an autopsy, the true cause of
death could easily be missed if circumstantial evidence does not suggest a
non-natural death. The value placed on toxicological analysis adds to the
problems relating to diagnosis. The fact that a poisonous substance is found in
the tissue does not necessarily indicate that this was the cause of death. Such
a finding could indicate that the deceased was exposed to that poison, either
in the environment or in his workplace. Conversely, the opposite finding does
not mean that poison was not the cause of death, since death could be caused by
some extremely poisonous substances in such minute quantities as to defy
routine chemical analytical detection. In experimental animals the botulism
toxin (a bacterial toxin) can cause death in doses as small as 0,0001 mg/kg of
body mass. Some poisons are broken down so rapidly in the body that the
metabolites cannot be identified; others are present in the tissues as normal
elements and only relatively small additional quantities may cause death,
particularly if given intravenously. Potassium chloride used as a resuscitative
drug to replenish tissue potassium after certain forms of cardiac collapse
could have disastrous consequences if administered incorrectly. Yet, on
analysis the blood potassium levels may have returned to normal at the time of
death a little while later. Various remedies are used by herbalists and
medicine men for a variety of ailments. The pharmacologically active substances
in these preparations are not always chemically identifiable.
Certain preparations are made from the wing
cases of the Cantharides beetle (Spanish fly), and concoctions are also made
from the bulb of the candelabra flower (Buphanedisticha). The use of
Cantharides as an abortifacient and an aphrodisiac has led to fatal poisoning,
as have concoctions made from the bulb of Buphanedisticha, given to adults for
a variety of complications.
Understandably a death suspected to have been
the result of poisoning may only be brought to the notice of the appropriate
authorities a considerable time later. This could necessitate an exhumation, in
which case special precautions (in addition to the standard precautions) have to
be taken when sampling for poisons. While care must be taken to avoid
contamination of samples by extraneous chemical substances, steps must also be
taken to identify possible contamination after burial by sampling the soil
above and below the body, as well as the shrouds and the coffin.
Case studies
1.
During a six-week period in 1969 seven young children died. Their
illness was heralded by fever, vomiting and diarrhoea, followed by severe liver
and kidney failure. Despite intensive medical supportive therapy, death ensued
within four days of admission to hospital. Initially the illness was thought to
be a ``natural disease'', probably viral in origin. An autopsy (not
medico-legal) was undertaken to confirm the clinical diagnosis. However, the
findings of a microscopic examination of tissues sampled at the autopsy were
suggestive of diethylene glycol poisoning. Epidemio-logical studies revealed a
single common factor in all the cases, namely a proprietary brand of paediatric
sedative mixture with a pharmaceutical formulation which included propylene
glycol as a solvent for the active ingredients. An analysis of this medicine
taken from the homes of the victims established that these medicines did not
contain propylene glycol, but diethylene glycol - a related highly toxic anti-freeze agent used
in engine-cooling systems. The source of the diethylene glycol was a drum
(incorrectly) labelled propylene glycol, which contained diethylene glycol.
This had been supplied to the manufacturing pharmaceutical company by the
importers as propylene glycol.
2.
In contrast with (1) above the death of a young male in 1977 following
on vomiting, delirium, jaundice, kidney failure and widespread tissue
haemorrhages was initially considered to have probably been the result of
poisoning. A medico-legal autopsy was therefore performed by Professor N
Scheepers. Microscopic examination of the tissues sampled at the autopsy
suggested that the condition was probably viral in origin. Further virological
studies subsequently confirmed this diagnosis; it was a case of haemorrhagic
fever caused by the Marburg virus. This was the first case reported in South
Africa, and the second series of cases in the world.
3.
A party of forty-five adult males was given an ointment containing
mercury, then commonly known as ``blue-butter'' and formerly used for treating
pubic lice infestation. The week's supply of ointment was (contrary to
instructions) enthusiastically rubbed into the pubic area that same evening by
forty of the ``patients'', who all became acutely ill within 12 hours with signs
of mercury poisoning, including nausea, burning sensation in the chest,
salivation, followed by a loosening of teeth in the jaw, and kidney
disturbances. Mercury was isolated in their urine samples. All of them later
developed the typical blue-line-on-the gum margins. Specific antidote treatment
was instituted, and after a ``stormy passage'' all the patients recovered. A
variety of toxic substances (and medica-ments) can be readily absorbed through
the skin; amongst these are mercury and various nitrites, such as TNT. Five
patients who were not poisoned had either not used the ointment, or had used it
according to instructions.
4.
A middle-aged company director was admitted to hospital, acutely shocked
and with severe abdominal pain and vomiting. A year earlier he had been treated
for a peptic ulcer. An emergency operation was considered necessary for a
suspected perforation of the ulcer. The patient died while still under general
anaesthetic and before the abdomen could be opened. In terms of the provisions
of the Health Professions Act relating to death while under, or in consequence
of a general or local anaesthetic, a medico-legal autopsy was performed. At the
autopsy the stomach lining had a velvety appearance, and a large subendocardial
haemorrhage was observed in the left ventricle of the heart. No other
significant signs which could account for death were found. The sub-endocardial
bleeding necessitated chemical analysis of the organs. Large quantities of
arsenic were discovered, enough to cause acute poisoning. The source of the
poison was never found, but in the light of circumstantial evidence, suicide
was suspected.
5.
An asthmatic patient also suffering from high blood pressure was issued
with a prescription for an anti-hypertensive medicine, containing an
adrenalin-blocking agent, in small therapeutic quantities. Within minutes of
taking the first dose the patient suffered an acute attack of asthma which did
not respond to the adrenalin-like anti-asthmatic medicine she had been
accustomed to use, since the former blocked the cellular receptor sites for the
latter. The patient died in status asthmaticus despite having been rushed to
hospital, and despite the expeditious application of resuscitative measures.
6.
The deceased, a political defector form Eastern Europe, felt something
sting him on the back of his thigh whilst waiting for a bus in London. On
reaching home his suspicion that a wasp had stung him was ``confirmed'' by the
discovery of a small puncture wound in the centre of a large inflamed area of his
thigh. He mentioned that he had noticed a man with a furled umbrella hurrying
away from the scene shortly after he had been stung. At the subsequent autopsy
a few days later a very small object which resembled a ball-bearing through
which a minute hole had been bored was found in the depths of the affected
tissues. It was later established that another defector in Paris had had a
similar experience but had not succumbed despite a stormy passage in hospital.
He was traced, his leg X-rayed and a similar object was revealed to be embedded
in the leg. This was removed, and both objects were identified as being of the
same composition and dimensions, and peculiar to an alloy used in the country
from which the two victims hailed. Subsequently it was established that the
hole in the object contained ricin in a concentrated form. The substance had
been the subject of research by a scientist in the aforementioned country.
Available evidence suggested that the furled umbrella was a cover for an
airgun-type weapon. The volume of ricin in the hole constituted a possible
lethal dose.
Post-mortem examination
In addition to the above signs of poisoning, it
is also important to submit the relevant specimens for toxicological analysis
during the post mortem. Blood, kidneys and urine, the liver and the stomach and
stomach contents will be routinely analysed. In some cases eye fluid or
vitreous humour (for alcohol) and other organs such as the brain, will also be
analysed. Hair and nails will also be examined especially in heavy metal
poisoning.
Related Topics