Chapter: Modern Pharmacology with Clinical Applications: Drugs Used in Dermatological Disorders
Topical Glucocorticosteroids
TOPICAL
GLUCOCORTICOSTEROIDS
Topical glucocorticosteroids
are the most widely pre-scribed drugs for skin diseases. Like systemic glucocor-ticosteroids,
topical glucocorticosteroids bind to cytoplasmic receptors that transport the
drug to the nucleus, where the complex binds to particular re-gions of DNA
known as the glucocorticoid response el-ement (GRE) and alters gene expression.
Such recep-tors have been identified in both epidermis and dermis.
Drug absorption is enhanced
by the use of agents with lipophilic side chains; by application of the drug to
larger areas of skin, to inflamed areas, and/or for long periods; and by the
use of occlusive dressings. Like their systemic counterparts, topical
glucocorticosteroids have myriad pharmacological effects. Especially important
in skin diseases are their antiinflammatory and immuno-suppressive effects and
their catabolic characteristics (hence their usefulness in eczematous
dermatitis and their toxicity of dermal atrophy, respectively).
Although their exact
mechanism of action is un-clear, they are known to inhibit the expression of
vari-ous cytokines and adhesion molecules and to antago-nize the activity of
transcription factors, including NF-B, NF-AT, and AP-1.
Topical corticosteroids are
most useful in inflamma-tory dermatoses, such as eczematous dermatitis and
pso-riasis; they may also be helpful in other skin diseases that have a prominent
inflammatory component, such as au-toimmune blistering diseases (e.g., bullous
pemphigoid and pemphigus vulgaris) and lupus erythematosus.
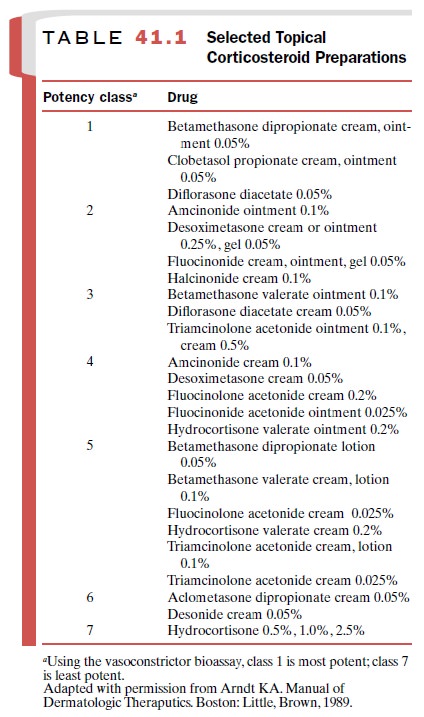
Many compounds are available
in both proprietary and generic forms, and their bioequivalence is difficult to
document. Nonetheless, the drugs are classified into seven categories according
to their relative potencies (Table 41.1).
Systemic toxicity from
topical corticosteroids can occur, particularly from the more potent agents.
Cushing’s syndrome, although rare, has been reported.
Milder suppression of the
hypothalamic–pituitary– adrenal axis is more common. Local toxicity is
relatively frequent and may not be reversible. Dermal atrophy, appearing as
striae or telangiectasias, is especially likely in intertriginous areas, where
occlusion occurs naturally and the skin is likely to be thin. Less commonly,
steroid-induced acneiform eruptions, rosacea, and perioral der-matitis can
occur. Glaucoma and cataracts have been reported from chronic application
around the eye. The normal inflammatory response to local infections may be
masked by corticosteroids, complicating diagnosis and therapy. Contact allergy
to the glucocorticosteroid preparations has been recognized with increasing
fre-quency. This may present as diagnostically confusing eczematous dermatitis
or unresponsiveness of the original dermatosis to treatment because the
steroid– allergen maintains partial antiinflammatory properties.
Related Topics