Chapter: Modern Pharmacology with Clinical Applications: Calcium Channel Blockers
Therapeutic Applications
THERAPEUTIC
APPLICATIONS
The calcium channel–blocking
drugs have been investi-gated for an unusually wide number of clinical
applica-tions. Verapamil-induced improvement of diastolic func-tion has proved
to be beneficial in the treatment of hypertrophic cardiomyopathy. Vasodilatory
properties of these drugs are used in the treatment of peripheral
vaso-constrictive disorders (Raynaud’s disease) and in reliev-ing vasospasm
following subarachnoid hemorrhage. There is ongoing interest in investigating
protective ef-fects on renal function and in the ability to reduce dele-terious
vascular changes in diabetes mellitus. Similarly, the potential benefit
afforded by their selective vasodila-tory action (especially the
second-generation agents) in the management of heart failure is an area of
interest. These drugs are of some benefit in a variety of noncar-diovascular
conditions characterized by hyperactivity of smooth muscle (e.g., achalasia).
However, their main ap-plications are as follows.
Hypertension
The calcium channel–blocking
drugs are effective anti-hypertensive agents and enjoy widespread use as single
medication or in combination. Their
effectiveness is re-lated to a decrease in peripheral resistance accompanied by
increases in cardiac index. The magnitude of their ef-fects is determined
partly by pretreatment blood pres-sure levels; maximum blood pressure lowering
gener-ally is seen 3 to 4 weeks after the start of treatment. These drugs
possess some distinct advantages relative to other vasodilators, including the
following:
·
Their relaxant effect on large arteries results in greater
compliance, which is beneficial in older persons.
·
Tolerance associated with renal retention of fluid does not occur;
an initial natriuretic effect is often observed, especially with the nifedipine
group of blockers.
·
They do not have significant effects on the re-lease of renin or
cause long-term changes in lipid or glucose metabolism.
·
Postural hypotension, first-dose effect, and re-bound phenomenon
are not commonly seen.
Their antihypertensive
efficacy is comparable to that of β-adrenergic blockers and angiotensin-converting
enzyme (ACE) inhibitors. The choice of a calcium chan-nel blocker, especially
for combination therapy, is largely influenced by the effect of the drug on
cardiac pacemakers and contractility and coexisting diseases, such as angina,
asthma, and peripheral vascular disease.
Ischemic Heart Disease
The effectiveness and use of
calcium channel blockers in the management of angina are well established ;
their benefit in postinfarction stages is less certain. Efficacy in angina is
largely derived from their hemodynamic effects, which influence the supply and
demand components of the ischemic balance (1) by in-creasing blood flow
directly or by increasing collateral blood flow and (2) by decreasing afterload
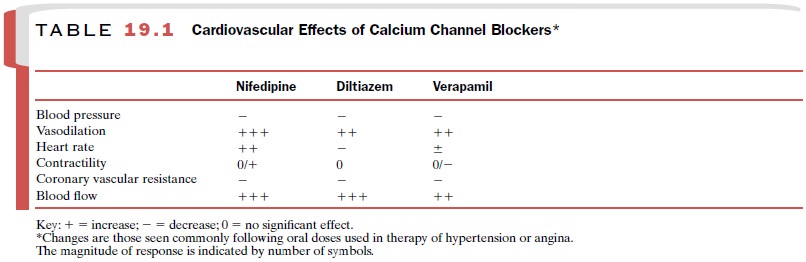
and reducing oxygen demand. All three
agents are useful in the man-agement of stable exertional angina, with
their vasodila-tory and cardiac effects making beneficial contributions. Given
the differences in their relative effects (Table 19.1), the response of the patient
can vary with the agent used and the preexisting cardiac status.
All agents are also effective in the control of variant
(Prinzmetal’s) angina, in which spasm of the coronary arteries is the main
factor. Their usefulness in the more complex
unstable (preinfarction) angina is less definite, depending on the hemodynamic
status and the suscep-tibility of the patient to infarction.
Cardiac Arrhythmias
The prominent depressant
action of verapamil and dil-tiazem at the SA and A-V nodes finds use in specific
ar-rhythmias. They are of proven efficacy
in acute control and long-term
management of paroxysmal supraventric-ular tachycardia .Their ability to
inhibit conduction at the A-V node is
employed in protecting ventricles from atrial tachyarrhythmias, often in
combi-nation with digitalis or propranolol.
Related Topics