Chapter: Essential Anesthesia From Science to Practice : Clinical management : Monitoring
The electroencephalogram and evoked responses - Anesthesia Clinical management
The electroencephalogram and
evoked responses
In
anesthesia, we expend much more effort in monitoring the cardiovascular and
respiratory system than the nervous system, even though anesthesia is all about
putting nervous function out of commission long enough to abolish awareness or
at least the perception of pain. The reason for our bias against monitoring
nervous activities is that we can afford to overdose the nervous functions and
put them completely to rest as long as we continue to satisfy the basal needs
for substrate and oxygen to brain and nerves. Hence, we worry more about the
circulation than about the brain. However, when the systemic circulation is
doing well but blood supply to all or parts of the brain or spinal cord is
threatened, we need to monitor their function. Two methods are available: the
electroencephalogram and evoked responses.
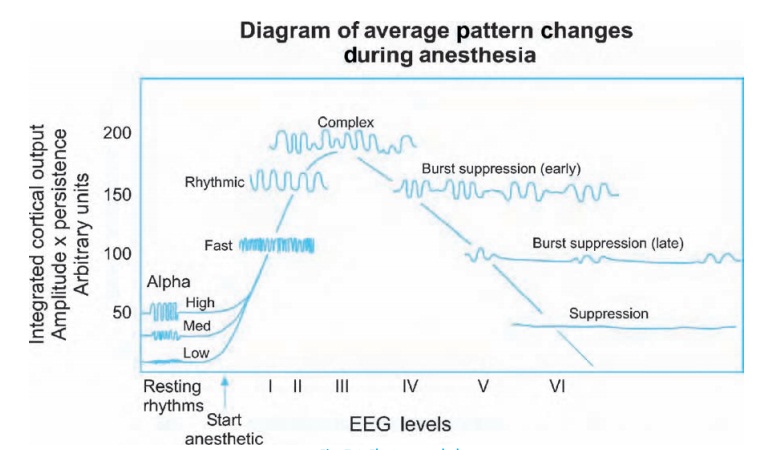
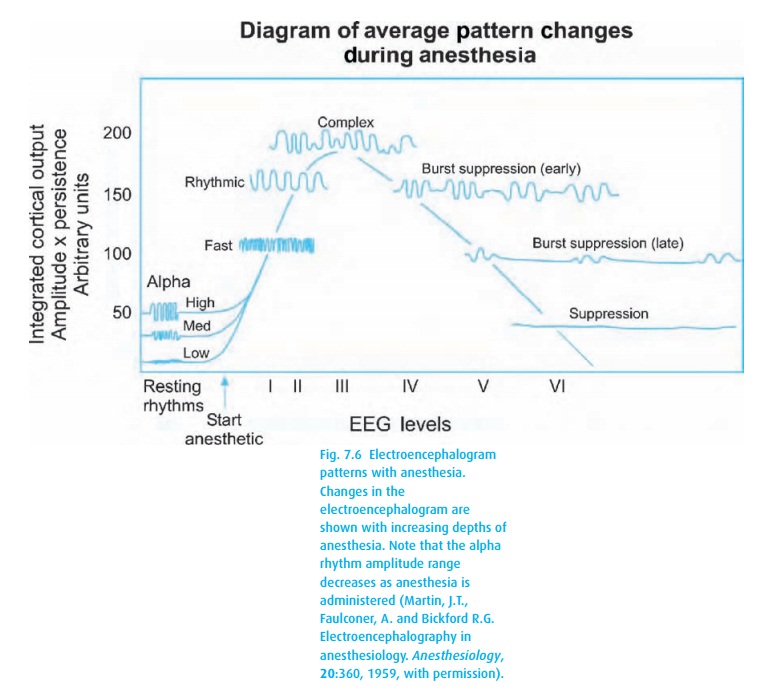
The EEG
as recorded by experts requires a montage with many electrodes. In anesthesia,
that is not practical and in the operating room, you will rarely see more than
a couple of leads plus a ground. The typical EEG of an awake individ-ual shows
rapid fire wiggles of low amplitude. With increasing depression of the central
nervous system, the frequency of the wiggles decreases, and the ampli-tude
increases. Before the EEG becomes flat, showing no electrical activity, it goes
through a stage of burst suppression in which brief electrical activity
alternates with longer periods of electrical silence. Figure 7.6shows these typical patterns which can be
described by the frequency of their waves and the amplitude of their
excursions.
The EEG can be processed to make interpretation more convenient. Several methods have been published. A commercial success has been the BIS (Bispec-tral index) monitor, which translates an automatic analysis of the EEG wave-forms (obtained from forehead leads) into a unit-less number between 0 and 100 – the higher the number, the more awake the patient. In general, a BIS of 60 or less is associated – most of the time – with general anesthesia. However, even in physiologic (not pharmacologic) sleep, the BIS can dip well below 60. Thus, we still need to consider the context (drugs, surgical stimulation) in which we observe BIS values. It will have served us well if it helps us to avoid exces-sively deep anesthesia – which might be harmful – and all too light anesthesia – which carries the risk of intraoperative awareness. Anesthesia that is neither too deep nor too light can speed postoperative recovery (wake-up and PACU time).
When we
need to monitor the integrity of specific neuronal pathways, we use the evoked
potential. Here, we apply a volley of either somatic, auditory, or visual
stimuli. The system then automatically scans the EEG, looking for responses to
the stimuli and filtering out all other activity in the EEG. It then presents
an evoked potential response with characteristic latencies and amplitude of
positive and negative deflections. Categorically, we can say that a central
response to a peripheral stimulus signifies that the sensory pathways between
periphery and brain are conducting impulses and that the brain is capable of
responding. If the response is delayed or muted, it is either because the
pathways have been affected or the brain is depressed, for example by
anesthetics. You can easily imagine that the monitoring of evoked responses can
be helpful when the integrity of the pathways are jeopardized by trauma or the
surgical intervention, e.g., scoliosis correction.
Related Topics