Chapter: Essential Anesthesia From Science to Practice : Clinical management : Monitoring
Monitoring respired gases - Anesthesia Clinical management
Monitoring respired gases
Capnography
The
delivery of carbon dioxide to the lungs depends first on the metabolic
production of carbon dioxide. Capnography, therefore, says something about
metabolism which may be depressed by cold or fired up during hyperthermia.
Capnography depends on blood flow to the lungs. It therefore says something
about circulation, specifically that regarding pulmonary blood flow. The
delivery of carbon dioxide in the expired gas requires ventilation of alveoli
and trans-port of alveolar gas to the outside. Capnography therefore says
something about ventilation. Because the ambient air is free of carbon dioxide
(well, not com-pletely free with only about 0.03% in air), the appearance of
carbon dioxide in the inspired gas must mean that carbon dioxide is being added
to the gas or that the patient is re-inhaling the carbon dioxide he just
exhaled, for exam-ple from a breathing circuit with a defective valve that
causes the dead space in the circuit to increase. Thus, capnography, the
measurement of carbon di-oxide in the respired gas, really offers rich
information that is relatively easily acquired.
The
respired gases can be sampled for analysis by aspirating gas from the breathing
circuit or from the nose – should the patient be breathing spontaneously – and
then delivering it to an analyzer. This is called “side-stream” sampling. We
can also clamp an analyzing cuvette directly on the breathing tube so that all
the respired gas passes through a system measuring the carbon dioxide, the
so-called “on-airway” or “main stream” capnogram.
There
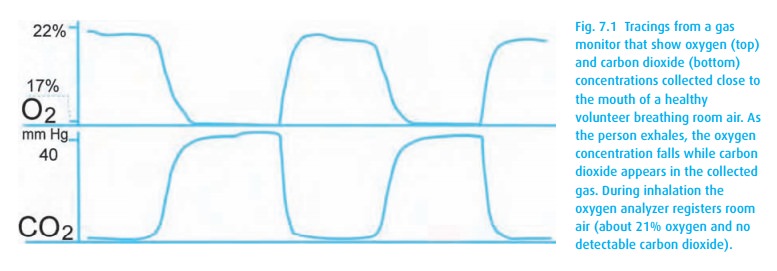
are several methods that enable us to measure carbon dioxide. Clin-ically most
often used are infra-red spectroscopy and chemical analysis. Because the
infra-red method responds rapidly, it is possible to generate a tracing of the
changing carbon dioxide concentration in the respired gases. A capnogram
results (Fig. 7.1).
The
chemical method is slow but can record approximate ranges of carbon dioxide in
gas, which is good enough if you are only interested whether CO2 is
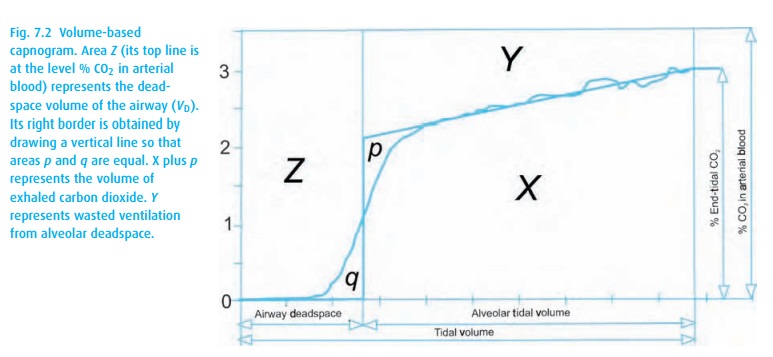
One
clever method, the volume-based capnogram, plots carbon dioxide over the volume
of gas exhaled (Fig. 7.2). It not only lets
us estimate the end-tidal concentration of carbon dioxide but it also provides
an estimate of deadspace.
Oxygen
When we
connect a patient to an atmosphere other than room air, we assume full
responsibility for the patient’s oxygen supply. The patient might require only
21% oxygen at ambient pressure at sea level, or he might need much more,
depending on clinical circumstances. Uncounted patients have died because that
seemingly simple requirement was not met either because gases were mixed such
that less than 21% oxygen was present in the inspired gas or because a gas
other than oxygen came out of the cylinder or pipeline as happens when
cylinders are misfilled or pipes delivering gases are switched by mistake.
Monitoring oxygen in the inspired gas, therefore, has become mandatory when
patients depend on us to prepare their respired gases.
Several
methods are available. Ideally, we would like to have a rapidly respond-ing
analyzer that generates “oxygrams” as shown in Fig. 7.1.
The technology for that relies on mass spectrometry or paramagnetic devices.
Many current anes-thesia machines incorporate a fairly slowly responding fuel
cell. However, even an instrument with a response time of many seconds
suffices.
Anesthetic gases
With
side-stream gas monitors, it becomes possible to use the technology
incorporated into capnography to analyze nitrous oxide and the halogenated
inhalation anesthetics. The response time of these analyzers enables us to
mon-itor both inspired and expired gas concentrations. We can thus watch what
con-centration the patient inhales. This frequently differs from the
concentration set at the vaporizer which delivers gas to the breathing circuit
where the fresh gases are diluted by the gases the patient re-inhales (see
Anesthesia machine chapter).
Temperature
The body
of an adult patient can absorb many calories before becoming notice-ably warmer
or, conversely, will cool only relatively slowly when losing heat by radiation
(which accounts for most of the heat loss), evaporation (next in impor-tance),
convection, and conduction (least important).2
However, monitoring the temperature, regardless how slowly it changes, becomes
important in babies and small children and in patients exposed to large heat
losses as occur with lengthy intraabdominal or intrathoracic operations. In
patients whose temperature drifts down to 35 °C, wound infections may be more
common. Other side effects of hypothermia include reduced enzyme activity and
shivering (which increases oxygen consumption potentially contributing to
myocardial ischemia), as well as the patient’s discomfort.
Central
blood in the vena cava or pulmonary artery gives the most representa-tive “core
temperature.” Tympanic membrane, esophagus, under the tongue, and the rectum
offer other sites. During endotracheal anesthesia, esophageal temper-atures can
be measured easily with the help of an esophageal stethoscope that carries a
temperature probe (thermistor) at its tip.
Skin
temperatures can be measured in the axilla and on the forehead. For the latter
site, temperature sensing adhesives are available that change their color with
changing temperatures. Their accuracy is limited not only by the fact that
ambient temperatures affect skin temperature but also because the
temperature-sensitive liquid crystals do not offer good resolution.
Related Topics