Chapter: The Massage Connection ANATOMY AND PHYSIOLOGY : Digestive System
The Structure and Function of Individual Organs of the Digestive System
The Structure and Function of Individual Organs of the Digestive System
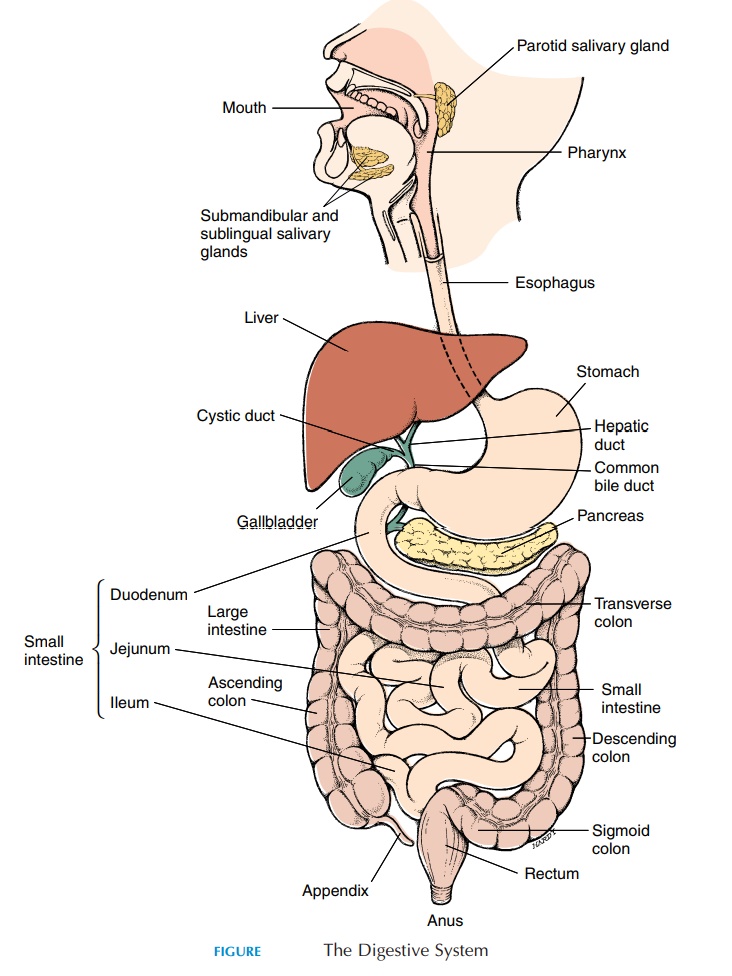
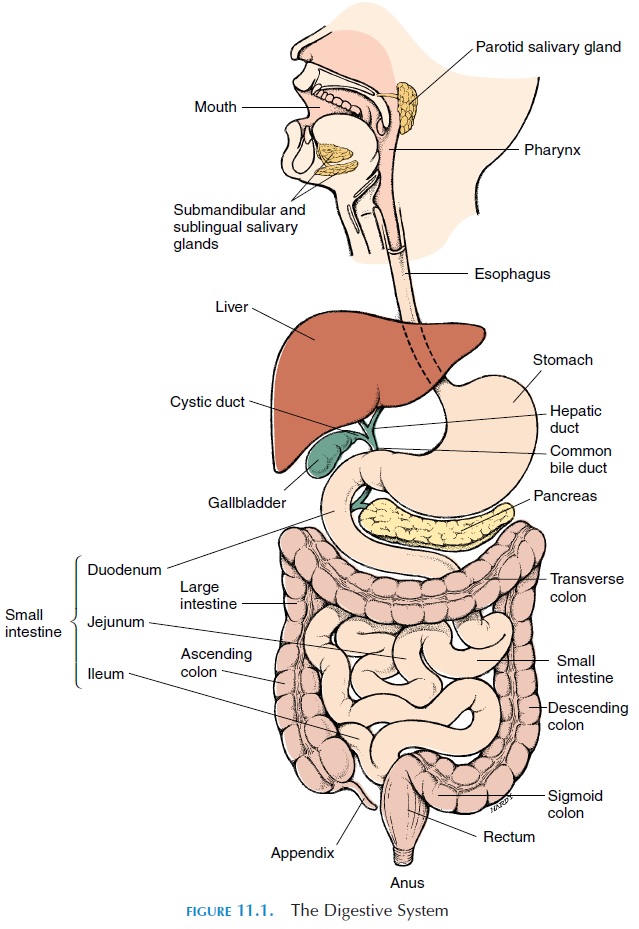
The digestive tract can be thought of as a very long tube, beginning in the mouth and ending in the anus. The tube is modified in different areas to fulfill spe-cific functions. Numerous accessory organs in and close to this tube help fulfill these functions. Figure 11.1 illustrates the principal organs of the digestive system. In this section, the digestive system will be described according to the path of food from the mouth to the anus.
THE MOUTH AND ASSOCIATED STRUCTURES
The mouth (see Figure 11.5) opens into the oral cavity, or buccal cavity. Anatomically, the mouth extends from inside the lips to the fauces, a constriction or nar-rowed area that can be seen in the back of the mouth. Beyond this, is the pharynx. The roof of the mouth is formed by the palate. The anterior two-thirds, the hard palate, is hard, containing bone. The posteriorone-third, the soft palate, has muscle and no bone and is, therefore, soft. The conical downward projection from the soft palate is known as the uvula. The soft palate and the uvula project backward from the hard palate and separate the pharynx into the oropharynx andnasopharynx. They prevent food from entering the nose during swallowing by closing the opening be-tween the nasopharynx and oropharynx.
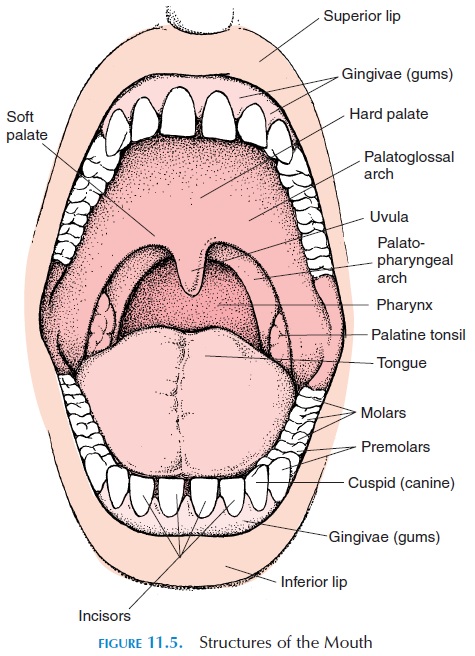
The fauces, or the posterior region of the mouth, has two mucosal arches on each side. Going from the palate toward the tongue is the palatoglossal arch, and behind it, going toward the pharynx, is the palatopharyngeal arch. When a person gags, themuscles in the two arches contract and narrow the opening between the mouth and the pharynx, a protective mechanism that prevents unwanted ob-jects from entering the digestive tract.
Between the two arches in the side, lie the palatinetonsils. The tonsils are part of the lymphoid system,and they help filter bacteria and toxins that may enter through the mucosa (inner lining) of the mouth.
The Teeth
The teeth (see Figure 11.6) are important for break-ing the food into small pieces. This process is known as mastication. The teeth arise from alveoli, small sockets in the mandibular and maxillary bones. The tooth is surrounded at the base by the gums, or gingivae.the bulk of each tooth is a bone-like material called dentin, which covers a cavity at the center of thetooth called the pulp cavity. Blood vessels and nerves pass through a canal (root canal) at the base (root) of the tooth to enter the pulp cavity. Collagen fibers (peridontal ligament), from the root of the tooth to the bone, hold the tooth in place.
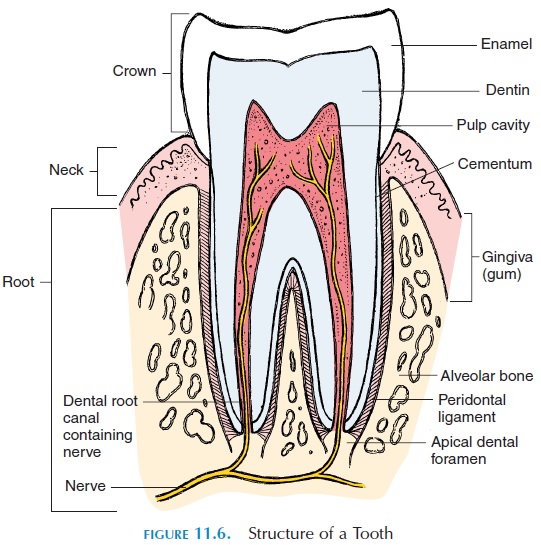
The ligament is re-inforced to the bone by cementum. The crown of the tooth is the portion visible above the gums. The dentin of the crown is covered by a layer of enamel, which is a crystalline form of calcium phosphate.
The teeth are modified according to function; four types have been identified. The blade-like incisors, found in the center of the mouth, cut, clip, and nip. The cuspids, orcanines—conical, with a sharp ridge and pointed tip—slash and tear. The bicuspids, or premolars, with flattened crowns and prominentridges, help crush, mash, and grind food. The poste-riorly located molars, larger versions of the bicuspids, crush and grind. In an adult, there are 3 pairs of molars, 2 pairs of bicuspids, 1 pair of cuspids, and 2 pairs of incisors in each jaw.
The cheeks, or lateral walls of the oral cavity, are comprised of the buccinator muscles and pads of fat. Anteriorly, the cheek is continuous with the lip, or labia. The space between the teeth and the cheeks isthe vestibule.
The Tongue
The tongue is muscular and has its own functions. It positions the food on the teeth, initiates swallowing, has taste buds that help taste food, and plays a key role in speech. The muscles of the tongue are con-trolled by the hypoglossal nerve (cranial nerve XII). Sensations such as touch, pain, and pressure are car-ried to the brain by the trigeminal nerve (cranial nerve V). The special sensation of taste is carried by the facial nerve, the glossopharyngeal nerve, and the vagus nerve. The facial nerve carries sensations from the anterior two-thirds of the tongue, and the glos-sopharyngeal carries it from the posterior one-third. The vagus nerve carries taste sensations from other areas of the mouth, such as the palate and pharynx.
The surface of the tongue appears fuzzy and has minute projections called papillae. Most of the taste buds—the sensory organs of taste—are located on the papillae. The taste buds have connections with nerve-endings that carry the sensation of taste to the brain. In humans, there are four basic tastes: sweet, sour, bitter, and salt. Bitter substances are best tasted on the back of the tongue; sour along the edges; sweet at the tip; and salt on the dorsum, anteriorly. Taste is sensed when the substances dissolved in the oral flu-ids come in contact with the taste buds.
SALIVARY GLANDS AND SALIVA
Adjacent to the mouth are many salivary glands (see Figure 11.7), which secrete about 1,500 mL (158.5 qt) of saliva per day. Saliva contains two enzymes that begin digestion of fat and carbohydrates. Mucins (glycoproteins) in the saliva lubricate thefood and protect the mucosa of the mouth. Some im-munoglobulins or antibodies are also present in the saliva as the first line of defense against bacteria and viruses. Other proteins that bind toxins, protect enamel (outer coating of teeth), and attack the walls of the bacteria are also present in the saliva.
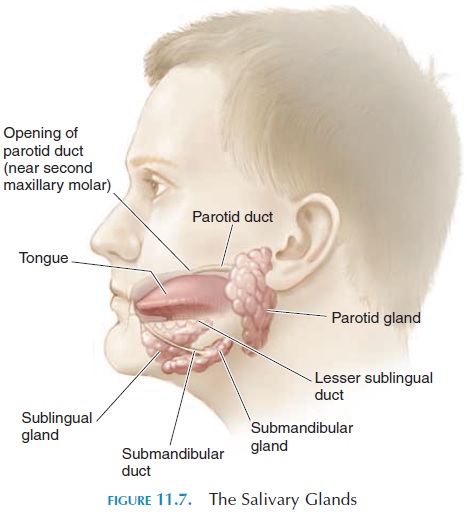
Saliva performs many important functions. Saliva makes swallowing easier, keeps the mouth moist, helps with speech by facilitating lip and tongue movement, keeps the mouth and teeth clean, and serves as a solvent for the molecules that stimulate taste sensations. Antibacterial properties are pro-vided to the saliva by antibodies and other proteins.
Salivary secretion is increased by stimulation of the autonomic nerves. Food in the mouth and lower end of the esophagus can increase secretion. It is well known that sight, smell, and even the thought of food can increase salivary production.
There are three pairs of salivary glands. The parotid glands are large and lie beneath the skin,covering the lateral and posterior aspect of the mandible (i.e., anterior to the ears). A duct from the parotid gland empties the saliva into the vestibule near the upper molar tooth. The sublingual glands are located in the floor of the mouth. Many ducts from this gland open under the tongue. The sub-mandibular glands are medial to the mandible onits inner surface, in the floor of the mouth.
PHARYNX
The pharynx is the common pathway for food and air and is connected to the nose, throat, and mouth. The pharynx extends from the posterior part of the nose to the entrance of the larynx and esophagus. It is di-vided into three regions—the nasopharynx, the oropharynx, and the laryngopharynx.
The nasopharynx lies above the soft palate and be-gins at the posterior part of the nasal cavity. Some lymphoid tissue—the pharyngeal tonsil—is located here. A tube from the middle ear, the eustachiantube, or pharyngotympanic tube, is found on eitherside. This tube equalizes the air pressure between the atmosphere and middle ear. The pressure has to be equal for normal hearing.
ESOPHAGUS
The esophagus (Figure 11.1) is a long tube that trans-ports food from the mouth to the stomach. It is about 25 cm (10 in) long and 2 cm (0.8 in) wide. It is located behind the trachea and travels downward in the pos-terior part of the thoracic cavity. Before it enters the abdomen, where the stomach is located, it passes through an opening in the diaphragm.
At the proximal end, closer to the pharynx, and at the distal end, closer to the stomach, circular muscles prevent entry of air and backflow of material from the stomach, respectively. The slight narrowing at the lower end of the esophagus is the lower esophagealsphincter. If this sphincter does not close properlyafter the food has entered the stomach, the stomach contents can regurgitate into the lower end of the esophagus. This condition is known as gastro-esophageal reflux disease. Because the contents ofthe stomach are acidic, the walls of the esophagus can become irritated and produce a burning sensa-tion in the epigastric region, referred to as heart-burn.
Swallowing
After mastication, food material is swallowed. The process of swallowing is known as deglutition. De-glutition is only voluntary at the start. Once the food material or bolus reaches the back of the mouth and touches the palatal arches, an involuntary reflex is triggered. The soft palate moves up, closing off the nasopharynx (you don’t breath when you swallow!), the larynx moves upward (have you noticed the thy-roid cartilage–Adam’s apple, bob up and down?), and the epiglottis moves back to close off the larynx and prevent food from entering the respiratory tract. The tongue moves up to the palate. In this way, all exits other than the esophagus are closed. As the food reaches the esophagus, a wave of peristalsis (the wave-like movement of the walls of the gut) occurs. In less than 9 seconds, the food is propelled into the stomach. Reverse peristalsis takes place when vomit-ing occurs.
STOMACH
The stomach is a sac-like, J-shaped expansion of the gut that stores the ingested food and propels the par-tially digested food into the intestines in smaller quantities. By churning movements, it further breaks down the food particles. The walls of the stomach have an abundance of smooth muscle that run circu-larly, obliquely, and longitudinally. Contraction of this muscle helps churn the food.
Enzymes (pepsin and gastric lipase) and acid (hy-drochloric acid) secreted by the glands in the walls of the stomach help break chemical bonds and partially digest the food. The acid kills many ingested bacteria and provides the right pH for pepsin to start protein digestion. Mucus, made up of glycoproteins and se-creted by mucous glands, protects the stomach wall from getting digested. The glands also produce a compound known as the intrinsic factor. Intrinsic factor is required for absorption of vitamin B12 in the small intestine. A total volume of about 2,500 mL (2.6 qt) of gastric juice is secreted per day.
The stomach is divided into specific regions (see Fig-ure 11.8). The cardia is the proximal region, close to the esophagus. The fundus is the portion of the stom-ach that is superior to the junction with the esophagus. The body is the area from the fundus to the curve of the J. The pylorus is the area of the curve of the J; it narrows into thepyloric canal before it opens into the first part of the intestine, the duodenum.
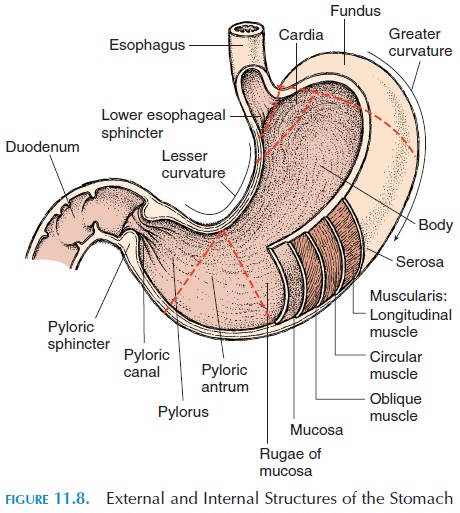
Circular muscles—the pyloric sphincter—guard the opening and regulate the amount of food mate-rial that enters the duodenum. The consistency of food is changed by the end of the processing by the stomach; watery and acidic, it is known as chyme.
The activity of the stomach, similar to the rest of the gut, is controlled by the central nervous system, local nervous reflexes, and gastrointestinal hor-mones. The gastric secretion increases with the sight, smell, taste, and even thought of food. Other emo-tions, such as anger, can increase secretions. Fear, anxiety, and stress can reduce the activity. Impulses from the brain reach the gut via the vagus nerve (cranial nerve X). When food arrives in the stomach, se-cretions are increased by the distension of the stom-ach, presence of undigested material, and pH changes. Food in the intestine has a feedback effect on the rate at which chyme is expelled into the intes-tine from the stomach. Details of the control mecha-nisms are beyond the scope of this book but, in short, nerves, local hormones, and local effects superim-posed by the central nervous system and hormones secreted elsewhere control the activity.
Digestion of proteins begins in the stomach. The digestion of carbohydrates and lipids that began in the mouth continues in the stomach until the pH drops (becomes acidic). The lining of the stomach is not conducive to food absorption. Few substances such as ethyl alcohol, some water, ions, short-chain fatty acids, and certain drugs (e.g., aspirin) are ab-sorbed here. The major part of digestion and absorp-tion occurs in the small intestine.
SMALL INTESTINE
The small intestine is a long tube approximately 3 m (9.8 ft) long and less than 2.5 cm (1 in) wide. A major part of the abdominal cavity is, therefore, occupied by the small intestine, with the liver occupying the upper right quadrant of the abdomen and the stom-ach, the epigastric region. About 90% of absorption occurs in the small intestine.
The intestine is divided into three parts: the duo-denum, the jejunum, and the ileum. The duodenum is the first part of the small intestine, leading off from the stomach. It is C-shaped, with the pancreas nes-tled in the curve of the C. The liver is located superior and lateral to the duodenum. Bile secretions from the liver, after being temporarily stored in the gallblad-der, flow into the duodenum.
The duodenum, unlike the rest of the small intes-tine, does not float freely in the abdominal cavity sus-pended by the mesentery. Instead, the duodenum is in close contact with the posterior part of the ab-domen at levels of L1 and L4 and is considered retroperitoneal (behind the peritoneum).
The jejunum, which is continuous with the duode-num, is 1 m (3.3 ft) long. Most digestion occurs here. The ileum, the third region, is the longest at 2 m (6.6 ft). At its distal end, it has circular smooth muscles— the ileocecal valve. This area of circular smooth muscle regulates the amount of chyme that enters the cecum, the first part of the large intestine.
The walls of the small intestine have numerous in-testinal glands that continue the digestion of food and numerous glands that secrete hormones. About 1.8 liters (1.9 qt) of watery fluid is secreted in the in-testines. An abundance of mucus, secreted by the submucous glands, protects the walls of the gut from digestion by enzymes. Because sympathetic stimula-tion decreases secretion, the duodenum becomes more vulnerable to destruction by chyme and devel-opment of ulcers. This is one association between stress and peptic ulcers.
THE PANCREAS
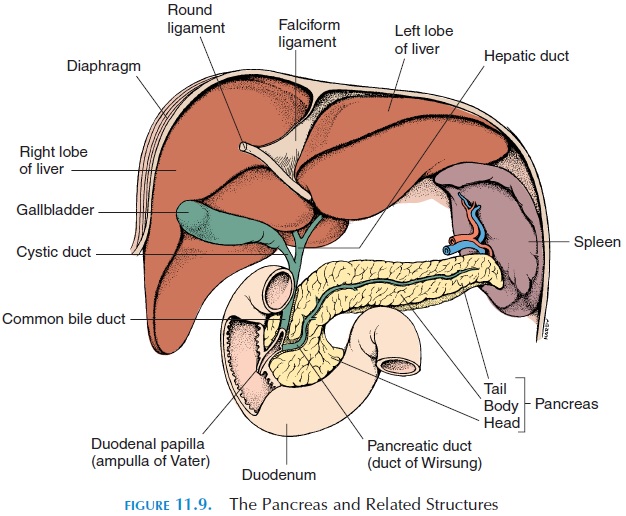
The pancreas (see Figure 11.9) is a gland that lies posterior to the stomach and to the left of the C-shaped curve of the duodenum. The end that lies in-side the curve of the C is larger and is known as the head. It tapers toward the other end, which extendsup to the spleen. This end is the tail of the pancreas, with the body in between.
The pancreas has two functions—exocrine and en-docrine. The exocrine function manufactures en- is the first part of the small intestine, leading off from the stomach. It is C-shaped, with the pancreas nes-tled in the curve of the C. The liver is located superior and lateral to the duodenum. Bile secretions from the liver, after being temporarily stored in the gallblad-der, flow into the duodenum.
The duodenum, unlike the rest of the small intes-tine, does not float freely in the abdominal cavity sus-pended by the mesentery. Instead, the duodenum is in close contact with the posterior part of the ab-domen at levels of L1 and L4 and is considered retroperitoneal (behind the peritoneum).
The jejunum, which is continuous with the duode-num, is 1 m (3.3 ft) long. Most digestion occurs here. The ileum, the third region, is the longest at 2 m (6.6 ft). At its distal end, it has circular smooth muscles— the ileocecal valve. This area of circular smooth muscle regulates the amount of chyme that enters the cecum, the first part of the large intestine.
The walls of the small intestine have numerous in-testinal glands that continue the digestion of food and numerous glands that secrete hormones. About 1.8 liters (1.9 qt) of watery fluid is secreted in the in-testines. An abundance of mucus, secreted by the submucous glands, protects the walls of the gut from digestion by enzymes. Because sympathetic stimula-tion decreases secretion, the duodenum becomes more vulnerable to destruction by chyme and devel-opment of ulcers. This is one association between stress and peptic ulcers.
THE PANCREAS
The pancreas (see Figure 11.9) is a gland that lies posterior to the stomach and to the left of the C-shaped curve of the duodenum. The end that lies in-side the curve of the C is larger and is known as the head. It tapers toward the other end, which extendsup to the spleen. This end is the tail of the pancreas, with the body in between.
The pancreas has two functions—exocrine and en-docrine. The exocrine function manufactures en-
The liver is covered by a tough connective tissue cap-sule over which is the peritoneum.
Unique Blood Supply to the Liver
The liver receives one third of its blood supply via the hepatic artery (see Figure ••), whose blood is derived from the aorta. The remaining two thirds comes from the hepatic portal vein, which drains blood from the esophagus, stomach, spleen, small intestine, and most of the large intestine. In this way, nutrients ab-sorbed from the gut are processed by the liver before they enter the general circulation. After processing in the liver, the blood enters the inferior vena cava via the hepatic vein.
An Overview of the Microscopic Structure of the Liver
The liver is made up of specialized cells called hepato-cytes. These cells are arranged in single file similar tothe spokes of a wheel (see Figure 11.10). At the center of the wheel is the central vein, which joins other cen-tral veins to form the hepatic vein. In the periphery of the wheel, are the blood vessels and ducts for bile. The blood vessels, branches of the hepatic artery (contain-ing oxygenated blood from the aorta) and the hepaticportal vein (containing blood from the gut, rich in nu-trients), open into sinusoids (large blood vessels) be-tween the line of hepatocytes. The sinusoids run paral-lel to the hepatocytes and open into the central vein.
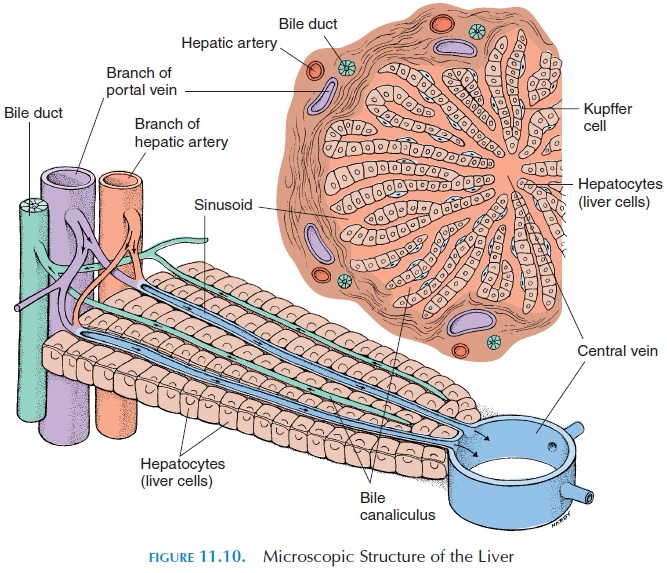
Other cells, Kupffer cells, are located in the walls of the sinusoids. Kupffer cells are actually macrophages (white blood cells), which destroy microorganisms that may have entered the blood through the gut.
Tiny channels that carry bile are found between the hepatocytes, along the spokes of the wheel. These channels open into the bile ductules located in the pe-riphery of the wheel. The bile ductules ultimately form the common hepatic duct that leaves the liver to join the duct from the gallbladder (cystic duct). The cystic duct and common hepatic duct join to form the com-mon bile duct, which opens into the duodenum.
From this description, it can be understood that the liver has an efficient architecture to fulfill its many functions.
Functions of the Liver
Physiology textbooks state that the liver has more than 200 different functions. The most important functions are discussed here. The liver is arranged in such a way that it can screen the blood going into the systemic circulation and adjust the levels of various substances in the blood.
Effect on carbohydrates: The liver helps main-tain the blood glucose level. It stores glucose ob-tained from the gut as glycogen, if the blood level of glucose is too high. If the glucose level drops, the glycogen is converted to glucose to return the blood glucose level to normal. Lipids and proteins are also used to manufacture glucose.
Effect on lipids: Similar to carbohydrates, theliver adjusts lipid levels in blood by mobilizing or storing lipids.
Effect on proteins: Amino acids absorbed fromthe gut may be stored in the liver for conversion into lipids, carbohydrates, or proteins. When needed, they are broken down. Ammonia is formed when amino acids are broken down. The liver converts the ammo-nia into urea, which is later excreted by the kidneys.
The liver manufactures most of the plasma pro-teins such as albumin, proteins required for the clot-ting process, and proteins used as transport vehicles in the blood. The liver also removes antibodies from the blood.
Removal of waste products: The liver detoxifiestoxins and drugs. Many drugs are rapidly converted to ineffective forms by the liver. That is why certain drugs must be given in larger quantities and in fre-quent doses. Conversely, dosage must be reduced in liver failure.
Removal of pathogens: The Kupffer cells, whichare fixed macrophages, remove pathogens and old and damaged blood cells. The breakdown product of hemoglobin (from red blood cells) —bilirubin—is re- moved from the blood and secreted into the bile for disposal.
Removal of circulating hormones: The liver is im-portant role for removing hormones that circulate in the blood, such as epinephrine, norepinephrine, thy-roid hormones, corticosteroids, and sex hormones.
Formation of vitamin D: One important functionof the liver is to convert a precursor of vitamin D that is manufactured in the skin or absorbed in the gut into an intermediary product that can be acted upon by the kidney. The kidney is the organ that finally forms vitamin D—one of the hormones that regulates calcium levels in the blood .
Storage of vitamins: The liver stores many vita-mins, especially vitamin B12 and the fat-soluble vita-mins, A, D, E, and K.
Mineral storage: An important mineral stored bythe liver is iron.
Bile synthesis: The liver manufactures bile, thesecretion vital for fat digestion and absorption. Bile is a yellow liquid that is mostly water. The most impor-tant component of bile is bile salts.
Because fat in the diet is not water-soluble, it coa-lesces to form large drops of fat in the gut. This makes it difficult for the enzymes secreted by the pancreas to act on the fat located deep inside the drop. The bile salts break the large drops into smaller ones, making it easier for the enzymes to act. In ad-dition, the bile salts facilitate the action of the en-zymes and help with the absorption of lipids through the mucosa into the body. Most bile salts that enter the gut via the bile duct are reabsorbed into the cir-culation and recycled by the liver.
Other than bile salts, bile also contains the bilepigment bilirubin, which is a breakdown product ofhemoglobin.
GALLBLADDER
The gallbladder (Figure 11.9) is a pear-shaped organ in close contact with the inferior surface of the liver. The cystic duct of the gallbladder joins with the com-mon hepatic duct to form the common bile duct. The function of the gallbladder is to store and concentrate bile that is secreted by the liver. The capacity of a normal gallbladder is about 40–70 mL (1.4–2.4 oz). Because the opening (sphincter) of the common bile duct is closed other than at meal times, the bile that is secreted by the liver is stored in the gallbladder.
When stored, some water from the bile is absorbed by the walls of the gallbladder, concentrating it. Con-traction of the smooth muscles of the gallbladder and opening of the sphincter is largely caused by chole-cystokinin, a hormone secreted by cells in the duo-denum.
ABSORPTION IN THE SMALL INTESTINE
The absorption is addressed in detail according to food type following the description of the rest of the digestive tract. The small intestine is fully suited for its absorptive function in that its length, presence of villi, and microvilli greatly increase the surface area. Also, the movement of the food material through it is quite slow—about 5 hours for food to pass from the duodenum to the end of the small intestine. In addi-tion, the blood supply and lymphatic supply are ex-tensive.
THE LARGE INTESTINE
The large intestine is much wider than the small in-testine. The large intestine (Figure 11.1) is about 6.5 cm (2.6 in) wide and 1.5 m (5 ft) long. The end of the ileum, guarded by the ileocecal valve (or sphincter), opens into the large intestine, which begins in the right lower quadrant of the abdomen. The large in-testine consists of three regions: the cecum, the colon, and the rectum. The rectum opens into theexterior via the anus. The main functions of the large intestine are to absorb water, sodium, and minerals from the chyme and make it more compact; absorb vitamins manufactured by the present bacteria; and, finally, to store fecal matter until it can be expelled from the body. The large intestine removes about 90% of the water in the chyme, reducing the 1–2 liters (1.1–2.1 qt) of chyme to 200–250 mL (about 0.2 qt) of feces passed per day.
The first part of the intestine—the cecum—has a small wormlike projection from the posteromedial side, the vermiform appendix. The appendix is about 7.5–15 cm (3–6 in) long, with a variable size and shape. It contains a large amount of lymphoid tissue. In hu-mans, it does not have an important function. Occa-sionally, the appendix becomes inflamed and produces the typical symptoms of appendicitis.
The colon can be subdivided into four parts—the ascending colon, the transverse colon, the de-scending colon, and the sigmoid colon—all namedaccording to their anatomy. The ascending colon as-cends from the right lower quadrant toward the liver in the posterior and lateral aspect of the abdominal cavity. Here, it makes a sharp bend, the hepatic flex-ure, to continue transversely as the transverse colonjust inferior to the stomach. To the left, it reaches the spleen before it bends inferiorly to continue as the descending colon. This bend is known as the splenicflexure. At the iliac fossa, the descending coloncurves inward and descends further as the sigmoid colon, the S-shaped segment of the large intestine. The sigmoid colon lies posterior to the urinary blad-der and becomes the rectum.
The rectum forms the last 15 cm (6 in) of the di-gestive tract. When food enters the rectum, there is an urge to defecate. The anus is the last few cen-timeters of the digestive tract. This region has circu-lar smooth muscles that form the internal analsphincter. Under voluntary control, the circularskeletal muscles located here form theexternal analsphincter.
The walls of the large intestine have cells that pro-duce large amounts of mucus. No enzymes are re-leased and no digestion occurs here. The longitudi-nally arranged smooth muscles in the walls of the colon form three bands called teniae coli. Because these longitudinal bands are shorter than the length of the colon, the wall of the colon forms outpouch-ings (haustra) between the teniae.
Feces
The feces contain inorganic material, undigested plant fibers, bacteria, and water. Surprisingly, a large fraction of the feces is of nondietary origin. Of the fe-ces, 75% is water and 25% is solids. Of the total solids, bacteria forms 30%; inorganic material, such as calcium and phosphate, 15%; fat and fat deriva-tives, 5%; and a variable amount of cellulose and in-digestible fiber, mucus, and mucosal cells that have sloughed off from the wall of the gut.
Bacteria and Colon
Although the jejunum contains little or no bacteria, the colon contains large numbers of bacteria. The bacteria in the colon are beneficial because many of them manufacture such vitamins as vitamin K and B complex. Chemicals formed by intestinal bacteria are largely responsible for the odor of the feces. Some bacteria residing in the intestine are harmful and may invade the body when the immunity is particu-larly low.
Dietary Fiber
Plant materials that reach the large intestine rela-tively unchanged are known as dietary fibers. Fibers are important to increase the bulk of the feces that is required to stretch the walls of the colon and initiate defecation. It has been shown that an intake of large amounts of vegetable fiber decreases the incidence of colon cancer, diabetes mellitus, and some types of heart diseases.
Related Topics