Chapter: Medical Surgical Nursing: Health Assessment
The Health History - Assessment
The Health History
Throughout assessment,
and particularly when obtaining the his-tory, attention is focused on the
impact of psychosocial, ethnic, and cultural background on the person’s health,
illness, and health-promotion behaviors. The interpersonal and physical
en-vironments, as well as the person’s lifestyle and activities of daily
living, are explored in depth. Many nurses are responsible for ob-taining a
detailed history of the person’s current health problems, past medical history,
family history, and a review of the person’s functional status. This results in
a total health profile that focuses on health as well as illness and is more
appropriately called a health history rather than a medical or a nursing
history.
The format of the health
history traditionally combines the medical history and the nursing assessment,
although formats based on nursing frameworks, such as functional health
patterns, have also become a standard. Both the review of systems and pa-tient
profile are expanded to include individual and family rela-tionships, lifestyle
patterns, health practices, and coping strategies. These components of the
health history are the basis of nursing as-sessment and can be easily adapted
to address the needs of any pa-tient population in any setting, institution, or
agency.
Combining the
information obtained by the physician and the nurse in one health history
prevents duplication of informa-tion and minimizes efforts on the part of the
person to providethis information. This also encourages collaboration among
members of the health care team who share in the collection and interpretation
of the data (Butler, 1999).
THE INFORMANT
The informant, or the
person providing the health history, may not always be the patient, as in the
case of a developmentally de-layed, mentally impaired, disoriented, confused,
unconscious, or comatose patient. The interviewer assesses the reliability of
the informant and the usefulness of the information provided. For example, a
disoriented patient is often unable to provide a reli-able database; people who
abuse drugs and alcohol often deny using these substances. The interviewer must
make a judgment about the reliability of the information (based on the context
of the entire interview), and he or she includes this evaluation in the record.
CULTURAL CONSIDERATIONS
When obtaining the
health history, the interviewer takes into ac-count the person’s cultural
background (Weber & Kelley, 2003). Cultural attitudes and beliefs about
health, illness, health care, hospitalization, the use of medications, and the
use of comple-mentary therapies are derived from each person’s experiences.
They vary according to the person’s ethnic and cultural back-ground. A person
from another culture may have a different view of personal health practices
than the health care practitioner.
Similarly, people from
some ethnic and cultural backgrounds will not complain of pain, even when it is
severe, because outward expressions of pain are considered unacceptable. In
some in-stances they may refuse to take analgesics. Other cultures have their
own folklore and beliefs about the treatment of illnesses. All such differences
in outlook must be taken into account and ac-cepted when caring for members of
other cultures. Attitudes and beliefs about family relationships and the role
of women and el-derly members of a family must be respected even if those
atti-tudes and beliefs conflict with those of the interviewer.
CONTENT OF THE HEALTH HISTORY
When the patient is seen
for the first time by a member of the health care team, the first requirement
is a database (except in emergency situations). The sequence and format of
obtaining data about the patient vary, but the content, regardless of format,
usually addresses the same general topics. A traditional approach includes the
following:
• Biographical data
• Chief complaint
• Present health concern (or present illness)
• Past history
• Family history
• Review of systems
• Patient profile
Biographical Data
Biographical information
puts the patient’s health history in con-text. This information includes the
person’s name, address, age, gender, marital status, occupation, and ethnic
origins. Some in-terviewers prefer to ask more personal questions at this part
of the interview, while others wait until more trust and confidence have been
established or until the patient’s immediate or urgent needs are first
addressed. The patient in severe pain or with another ur-gent problem is
unlikely to have a great deal of patience for an in-terviewer who is more
concerned about marital or occupational status than with quickly addressing the
problem at hand.
Chief Complaint
The chief complaint is
the issue that brings the person to the at-tention of the health care provider.
Questions such as, “Why have you come to the health center today?” or “Why were
you admit-ted to the hospital?” usually elicit the chief complaint. In the home
setting, the initial question might be, “What is bothering you most today?”
When a problem is identified, the person’s exact words are usually recorded in
quotation marks (Orient, 2000). However, a statement such as, “My doctor sent
me” should be followed up with a question that identifies the probable reason
why the person is seeking health care; this reason is then identified as the
chief complaint.
Present Health Concern or Illness
The history of the
present health concern or illness is the single most important factor in
helping the health care team to arrive at a diagnosis or determine the person’s
needs. The physical exami-nation is helpful but often only validates the
information obtained from the history. A careful history assists in correct
selection of ap-propriate diagnostic tests. While diagnostic test results can
be helpful, they often support rather than establish the diagnosis.
If the present illness
is only one episode in a series of episodes, the entire sequence of events is
recorded. For example, a history from a patient whose chief complaint is an
episode of insulin shock describes the entire course of the diabetes to put the
cur-rent episode in context. The details of the health concern or pres-ent
illness are described from onset until the time of contact with the health care
team. These facts are recorded in chronological order, beginning with, for
example, “The patient was in good health until . . .” or “The patient first
experienced abdominal pain 2 months prior to seeking help.”
The history of the
present illness or problem includes such in-formation as the date and manner
(sudden or gradual) in which the problem occurred, the setting in which the
problem occurred (at home, at work, after an argument, after exercise),
manifesta-tions of the problem, and the course of the illness or problem. This
includes self-treatment (including complementary therapies), medical
interventions, progress and effects of treatment, and the patient’s perceptions
of the cause or meaning of the problem.
Specific symptoms (pain,
headache, fever, change in bowel habits) are described in detail, along with
the location and radia-tion (if pain), quality, severity, and duration. The
interviewer also asks if the problem is persistent or intermittent, what
factors ag-gravate or alleviate it, and if any associated manifestations exist.
Associated
manifestations are symptoms that occur simultane-ously with the chief
complaint. The presence or absence of such symptoms may shed light on the
origin or extent of the problem, as well as on the diagnosis. These symptoms
are referred to as sig-nificant positive or negative findings and are obtained
from a re-view of systems directly related to the chief complaint. For example,
if the person reports a vague symptom such as fatigue or weight loss, all body
systems are reviewed and included in this sec-tion of the history. If, on the
other hand, the person’s chief com-plaint is chest pain, only the
cardiopulmonary and gastrointestinal systems may be included in the history of
the present illness. In either situation, both positive and negative findings
are recorded to define the problem further.
Past Health History
A detailed summary of
the person’s past health is an important part of the database. After
determining the general health status, the interviewer may inquire about
immunization status and any known allergies to medications or other substances.
The dates of immunization are recorded, along with the type of allergy and
ad-verse reactions. The person is asked to provide information, if known, about
his or her last physical examination, chest x-ray, electrocardiogram, eye
examination, hearing tests, dental checkup, as well as Papanicolaou (Pap) smear
and mammogram (if female), digital rectal examination of the prostate gland (if
male), and any other pertinent tests. Previous illnesses are then discussed.
Nega-tive as well as positive responses to a list of specific diseases are
recorded. Dates, or the age of the patient at the time of illness, as well as
the names of the primary health care provider and hospi-tal, the diagnosis, and
the treatment are also recorded. A history of the following areas is elicited:
·
Childhood illness—rubeola, rubella, polio, whooping
cough, mumps, chickenpox, scarlet fever, rheumatic fever, strep throat
·
Adult illnesses
·
Psychiatric illnesses
·
Injuries—burns, fractures, head injuries
·
Hospitalizations
·
Surgical and diagnostic procedures
·
Current medications—prescription, over-the-counter,
home remedies, complementary therapies
·
Use of alcohol and other drugs
If a particular
hospitalization or major medical intervention is related to the present
illness, the account of it is not repeated; rather, the report refers to the
appropriate part of the report, such as “see history of present illness” or
“see HPI” on the data sheet.
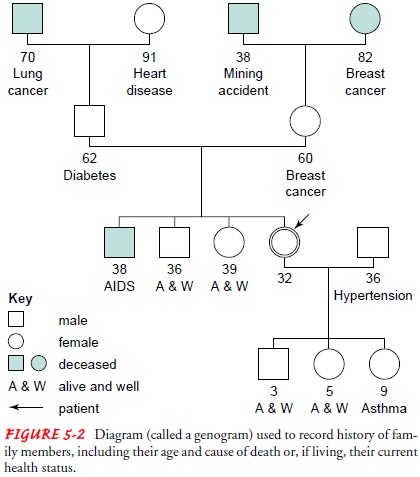
Family History
The age and health
status, or the age and cause of death, of first-order relatives (parents,
siblings, spouse, children) and second-order relatives (grandparents, cousins)
are elicited to identify diseases that may be genetic in origin, communicable,
or possi-bly environmental in cause. The following diseases are generally
included: cancer, hypertension, heart disease, diabetes, epilepsy, mental
illness, tuberculosis, kidney disease, arthritis, allergies, asthma,
alcoholism, and obesity. One of the easiest methods of recording such data is
by using the family tree or genogram (Fig. 5-2). The results of genetic testing
or screening, if known, are recorded.
Review of Systems
The systems review
includes an overview of general health as well as symptoms related to each body
system. Questions are asked about each of the major body systems in terms of
past or present symptoms. Reviewing each body system helps reveal any relevant
data. Negative as well as positive answers are recorded. If the pa-tient
responds positively to questions about a particular system, the information is
analyzed carefully. If any illnesses were previ-ously mentioned or recorded, it
is not necessary to repeat them in this part of the history. Instead, reference
is made to the appro-priate place in the history where the information can be
found.
A review of systems can be organized in a formal checklist, which becomes a part of the health history. One advantage of a checklist is that it can be easily audited and is less subject to error than a system that relies heavily on the interviewer’s memory.
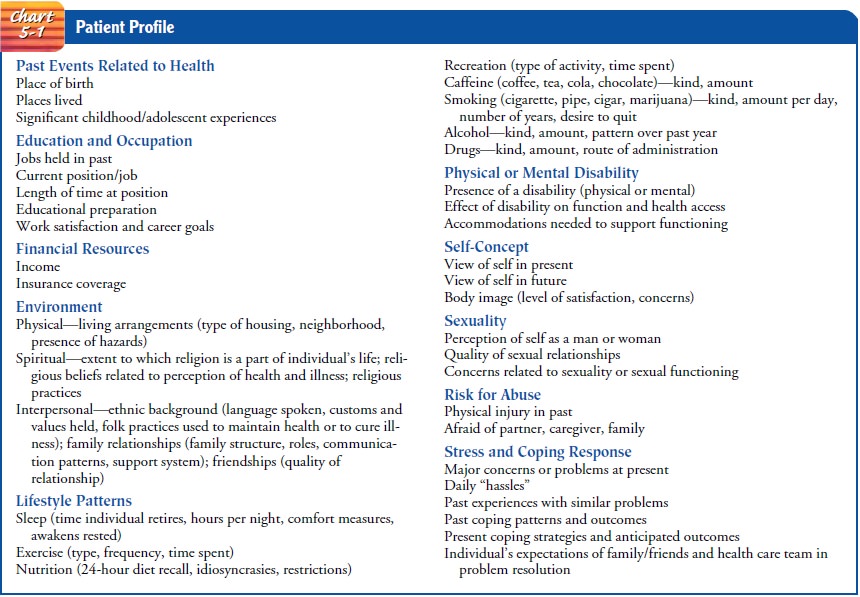
Patient Profile
In the patient profile,
more biographical information is gathered. A complete composite, or profile, of
the patient is critical to an analysis of the chief complaint and of the
person’s ability to deal with the problem. A complete patient profile is
summarized in Chart 5-1.
The information elicited
at this point in the interview is highly personal and subjective. During this
stage, the person is encour-aged to express feelings honestly and to discuss
personal experi-ences. It is best to begin with general, open-ended questions
and to move to direct questioning when specific facts are needed. The patient is
often less anxious when the interview progresses from information that is less
personal (birthplace, occupation, educa-tion) to information that is more
personal (sexuality, body image, coping abilities).
A general patient
profile consists of the following content areas:
• Past life events related to health
• Education and occupation
• Environment (physical, spiritual, cultural, interpersonal)
• Lifestyle (patterns and habits)
• Presence of a physical or mental disability
• Self-concept
• Sexuality
• Risk for abuse
• Stress and coping response
PAST LIFE EVENTS RELATED TO HEALTH
The patient profile begins with a brief life history. Questions about place of birth and past places of residence help focus at-tention on the earlier years of life. Personal experiences during childhood or adolescence that have special significance may be elicited by asking, “Was there anything that you experienced as a child or adolescent that would be helpful for me to know about?”
The interviewer’s intent
is to encourage the person to make a quick review of his or her earlier life,
highlighting information of particular significance. Although many patients may
not recall anything significant, others may share information such as a per-sonal
achievement, a failure, a developmental crisis, or an in-stance of physical or
emotional abuse.
EDUCATION AND OCCUPATION
Inquiring about current
occupation can reveal much about a per-son’s economic status and educational
preparation. A statement such as, “Tell me about your job” often elicits
information about role, job tasks, and satisfaction with the position. Direct
questions about past employment and career goals may be asked if the per-son
does not provide this information.
Asking the person what
kind of educational requirements were necessary to attain his or her present
job is a more sensitive approach to educational background than asking whether
he or she graduated from high school. Information about the patient’s general
financial status may be obtained by questions such as, “Do you have any
financial concerns at this time?” or “Sometimes there just doesn’t seem to be
enough money to make ends meet. Are you finding this true?” Inquiry about the
person’s insurance coverage and plans for health care payment is also
appropriate.
ENVIRONMENT
The person’s physical environment and its potential hazards, spir-itual awareness, cultural background, interpersonal relationships, and support system are included in the concept of environment.
Physical Environment
Information is elicited
about the type of housing (apartment, du-plex, single-family) in which the
person lives, its location, the level of safety and comfort within the home and
neighborhood, and the presence of environmental hazards (eg, isolation,
poten-tial fire risks, inadequate sanitation). The patient’s environment takes
on special importance if the patient is homeless or living in a homeless
shelter or has a disability.
Spiritual Environment
The term “spiritual
environment” refers to the degree to which a person thinks about or
contemplates his or her existence, accepts challenges in life, and seeks and
finds answers to personal ques-tions. Spirituality may be expressed through
identification with a particular religion. Spiritual values and beliefs often
direct a per-son’s behavior and approach to health problems and can influ-ence
responses to sickness. Illness may create a spiritual crisis and can place
considerable stress on a person’s internal resources and beliefs. Inquiring
about spirituality can identify possible support systems as well as beliefs and
customs that need to be considered in planning care. Thus, information is
gathered in the following three areas:
·
The extent to which religion is a part of the
person’s life
·
Religious beliefs related to the person’s
perception of health and illness
·
Religious practices
The following questions
can be used in a spiritual assessment:
· Is religion or God
important to you?
· If yes, in what way?
· If no, what is the most
important thing in your life?
· Are there any religious
practices that are important to you?
· Do you have any
spiritual concerns because of your present health problem?
Interpersonal and Cultural Environment
Cultural influences,
relationships with family and friends, and the presence or absence of a support
system are all a part of one’s in-terpersonal environment. The beliefs and
practices that have been shared from generation to generation are known as
cultural or ethnic patterns. They are expressed through language, dress,
di-etary choices, and role behaviors, in perceptions of health and ill-ness,
and in health-related behaviors. The influence of these beliefs and customs on
how a person reacts to health problems and interacts with health care providers
cannot be underestimated (Fuller & Schaller-Ayers, 2000). For this reason,
the health history includes information about ethnic identity (cultural and
social) and racial identity (biologic). The following questions may assist in
obtaining relevant information:
· Where did your parents
or ancestors come from? When?
· What language do you
speak at home?
· Are there certain
customs or values that are important to you?
· Is there anything
special you do to keep in good health?
· Do you have any specific
practices for treating illness?
Family Relationships and Support System
An assessment of family
structure (members, ages, roles), patterns of communication, and the presence
or absence of a support sys-tem is an integral part of the patient profile. Although
the tradi-tional family is recognized as a mother, a father, and children, many
different types of living arrangements exist within our so-ciety. “Family” may
mean two or more people bound by emo-tional ties or commitments. Live-in
companions, roommates, and close friends can all play a significant role in an
individual’s support system.
LIFESTYLE
The lifestyle section of
the patient profile provides information about health-related behaviors. These
behaviors include patterns of sleep, exercise, nutrition, and recreation, as
well as personal habits such as smoking and the use of drugs, alcohol, and
caffeine. Although most people readily describe their exercise patterns or
recreational activities, many are unwilling to report their smok-ing, alcohol use,
and drug use; many deny or understate the de-gree to which they use such
substances. Questions such as, “What kind of alcohol do you enjoy drinking at a
party?” may elicit more accurate information than, “Do you drink?” The specific
type of alcohol (eg, wine, liquor, beer) and the amount ingested per day or per
week (eg, 1 pint of whiskey daily for 2 years) are described.
When alcohol abuse is
suspected, additional information may be obtained by using common alcohol
screening questionnaires such as the CAGE (Cutting down, Annoyance by
criticism, Guilty feelings, and Eye-openers), AUDIT (Alcohol Use Disorders
Identification Test), TWEAK (Tolerance, Worry, Eye-opener, Amnesia, Kut down),
or SMAST (Short Michigan Alcoholism Screening Test). Chart 5-2 shows the CAGE
Questions Adapted to Include Drugs (CAGEAID).
Similar questions can be
used to elicit information about smoking and caffeine consumption. Questions
about drug use follow naturally after questions about smoking, caffeine
con-sumption, and alcohol use. A nonjudgmental approach will make it easier for
the person to respond truthfully and factually. If street names or unfamiliar
terms are used to describe drugs, the person is asked to define the terms used.
Investigation of
lifestyle should also include questions about complementary and alternative
therapies. It is estimated that as many as 40% of Americans use some type of
complementary or al-ternative therapies, including special diets, the use of
prayer, visu-alization, or guided imagery, massage, meditation, herbal
products, and many others (Evans, 2000; King, Pettigrew & Reed, 1999; Kuhn,
1999). Marijuana is used for symptom management, espe-cially pain, in a number
of chronic conditions (Mathre, 2001).
PHYSICAL OR MENTAL DISABILITY
The general patient
profile also needs to contain questions about any hearing, vision, cognitive,
or physical disability. The presence of an obvious physical deformity—for
instance, if the patient walks with crutches or needs a wheelchair to get
around—needs further investigation. The etiology of the disability should be
elicited; the length of time the patient has had the disability and the impact
on function and health access are important to assess.
SELF-CONCEPT
Self-concept refers to
one’s view of oneself, an image that has de-veloped over many years. To assess
self-concept, the interviewer might ask the person how he or she views life:
“How do you feel about your life in general?” A person’s self-concept can be
threat-ened very easily by changes in physical function or appearance or other
threats to health. The impact of certain medical conditions or surgical
interventions, such as a colostomy or a mastectomy, can threaten body image.
Asking, “Do you have any particular concerns about your body?” may elicit useful
information about self-image.
SEXUALITY
No area of assessment is
more personal than the sexual history. Interviewers are frequently
uncomfortable with such questions and ignore this area of the patient profile
or conduct a very cur-sory interview at this point. Lack of knowledge about
sexuality and anxiety about one’s own sexuality may hamper the inter-viewer’s
effectiveness in dealing with this subject (Ross, Channon-Little & Rosser,
2000).
Sexual assessment can be
approached at the end of the inter-view, at the time interpersonal or lifestyle
factors are assessed, or it can be a part of the genitourinary history within
the review of systems. For instance, it may be easier to approach a discussion
of sexuality after a discussion of menstruation. A similar discus-sion with the
male patient would follow questions related to the urinary system.
Obtaining the sexual
history provides an opportunity to dis-cuss sexual matters openly and gives the
person permission to express sexual concerns to an informed professional. The
inter-viewer must be nonjudgmental and must use language appropri-ate to the
patient’s age and background. It is advisable to begin the assessment with a
general question concerning the person’s developmental stage and the presence
or absence of intimate re-lationships. Such questions may lead to a discussion
of concerns related to sexual expression or the quality of a relationship, or
to questions about contraception, risky sexual behaviors, and safer sex
practices.
Finding out whether a person
is sexually active should precede any attempts to explore issues related to
sexuality and sexual func-tion. Care should be taken to initiate conversations
about sexuality with elderly patients and not to treat them as asexual beings
(Miller, Zylstra & Stranridge, 2000). Questions are worded in such a way
that the person feels free to discuss his or her sexual-ity regardless of
marital status or sexual preference. Direct ques-tions are usually less
threatening when prefaced with such statements as, “Most people feel that . .
.” or “Many people worry about. . . .” This suggests the normalcy of such
feelings or be-havior and encourages the person to share information that might
otherwise be omitted from fear of seeming “different.”
If the person answers abruptly
or does not wish to carry the dis-cussion any further, then the interviewer
should move to the next topic. However, introducing the subject of sexuality
indicates to the person that a discussion of sexual concerns is acceptable and
can be approached again in the future if so desired.
RISK FOR ABUSE
A topic of growing
importance in today’s society is physical, sex-ual, and psychological abuse.
Such abuse occurs at all ages, to men and women from all socioeconomic, ethnic,
and cultural groups (Little, 2000; Marshall, Benton & Brazier, 2000). Few
patients, however, will discuss this topic unless they are asked specifically
about it. Therefore, it is important to ask direct questions, such as:
· Is anyone physically
hurting you?
· Has anyone ever hurt you
physically or threatened to do so?
· Are you ever afraid of
anyone close to you (your partner, caretaker, or other family members)?
If the person’s response indicates that abuse is a risk, further assessment is called for and efforts are made to ensure the per-son’s safety and provide access to appropriate community and professional resources and support systems.
Further discussion of domestic violence and
abuse. When questioned directly, elderly patients rarely admit to abuse
(Marshall, Benton & Brazier, 2000). Health care professionals should assess
for risk factors, such as high levels of stress or al-coholism in caregivers,
evidence of violence, high emotions as well as financial, emotional, or
physical dependency. Patients who are elderly or disabled are at increased risk
for abuse and should be asked about it as a routine part of assessment.
STRESS AND COPING RESPONSES
Each person handles
stress differently. How well we adapt de-pends on our ability to cope. During a
health history, past cop-ing patterns and perceptions of current stresses and
anticipated outcomes are explored to identify the person’s overall ability to
handle stress. It is especially important to identify expectations that the
person may have of family, friends, and caregivers in pro-viding financial,
emotional, or physical support.
OTHER HEALTH HISTORY FORMATS
The health history
format discussed is only one pos-sible format that is useful in obtaining and
organizing information about a person’s health status. Some consider this
traditional for-mat to be inappropriate for nurses because it does not focus
exclu-sively on the assessment of human responses to actual or potential health
problems. Several attempts have been made to develop an assessment format and
database with this focus in mind. One ex-ample is the nursing database
prototype based on the North Amer-ican Nursing Diagnosis Association’s (NANDA)
Unitary Person Framework and its nine human response patterns: exchanging,
communicating, relating, valuing, choosing, moving, perceiving, knowing, and
feeling. Although there is support in nursing for using this approach, no
consensus for its use has been reached.
The National Center for
Health Services Research of the U.S. Department of Health and Human Services
and other groups from the public and private sectors have focused on assessing
not only biologic health but also other dimensions of health. These dimen-sions
include physical, functional, emotional, mental, and social health. Modern efforts
to assess health status have focused on the manner in which disease or
disability affects the patient’s functional status—that is, the ability of the
person to function normally and perform his or her usual physical, mental, and
social activities. An emphasis on functional assessment is viewed as more
holistic than the traditional health or medical history. Instruments to assess
health status in these ways may be used by nurses along with their own clinical
assessment skills to determine the impact of illness, dis-ease, disability, and
health problems on functional status.
Health concerns that are
not complex (earache, tonsillectomy) and can be resolved in a short period of
time usually do not require the depth or detail that is required when a person
is experiencing a major illness or health problem. Additional assessments that
go beyond the general patient profile may be used when the patient’s health
problems are acute and complex or when the illness is chronic. Individuals
should be asked about their continuing health promotion and screening
practices. Patients who have not been in-volved in these practices in the past
are educated about their im-portance and are referred to appropriate health
care providers.
Regardless of the
assessment format used, the nurse’s focus during data collection is different
from that of the physician and other health team members; however, it
complements these ap-proaches and encourages collaboration among the health
care providers, as each member brings his or her own expertise and focus to the
situation.
Related Topics