Chapter: Medical Surgical Nursing: Health Assessment
Nutritional Assessment
Nutritional Assessment
An additional area of
concern that is often integrated into the health history and physical
examination is an in-depth nutritional assessment. Nutrition is important to
maintain health and to pre-vent disease and death (Kant, Schatzkin, Graubard
& Schairer, 2000; Landi, Onder, Gambassi et al., 2000; Stampfer, Hu &
Manson, 2000). Disorders caused by nutritional deficiency, over-eating, or
eating poorly balanced meals are among the leading causes of illness and death
in the United States today. The three leading causes of death are related, in
part, to consequences of un-healthy nutrition: heart disease, cancer, and
stroke (Hensrud, 1999). Other examples of health problems associated with poor
nutrition include obesity, osteoporosis, cirrhosis, diverticulitis, and eating
disorders. When illness or injury occurs, optimal nu-trition is an essential
factor in promoting healing and resisting in-fection and other complications
(Braunschweig, Gomez & Sheean, 2000). Assessment of a person’s nutritional
status provides infor-mation on obesity, undernutrition, weight loss,
malnutrition, de-ficiencies in specific nutrients, metabolic abnormalities, the
effects of medications on nutrition, and special problems of the hospi-talized
patient and the person who is cared for in the home and in other community
settings.
Certain signs and
symptoms that suggest possible nutritional deficiency are easy to note because
they are specific. Other phys-ical signs may be subtle and must be carefully
assessed. A physi-cal sign that suggests a nutritional abnormality should be
pursued further. For example, certain signs that may appear to indicate
nutritional deficiency may actually reflect other systemic condi-tions (eg,
endocrine disorders, infectious disease). Others may re-sult from impaired
digestion, absorption, excretion, or storage of nutrients in the body.
The sequence of
assessment of parameters may vary, but eval-uation of nutritional status
includes one or more of the following methods: measurement of body mass index
(BMI) and waist cir-cumference; biochemical measurements (albumin, transferrin,
prealbumin, retinol-binding protein, total lymphocyte count, elec-trolyte
levels, creatinine/height index); clinical examination find-ings; and dietary
data.
BODY MASS INDEX
BMI is a ratio based on
body weight and height. The obtained value is compared to the established
standards; however, trends or changes in values over time are considered more
useful than isolated or one-time measurements. BMI (Fig. 5-6) is highly
correlated with body fat, but increased lean body mass or a large body frame
can also increase the BMI. Individuals who have a BMI below 24 (or who are 80%
or less of their desirable body weight for height) are at increased risk for
problems associated with poor nutritional status. In addition, a low BMI is
associ-ated with higher mortality rates in hospitalized patients and
community-dwelling elderly (Landi et al., 2000; Landi, Zuccala, Gambassi et
al., 1999).
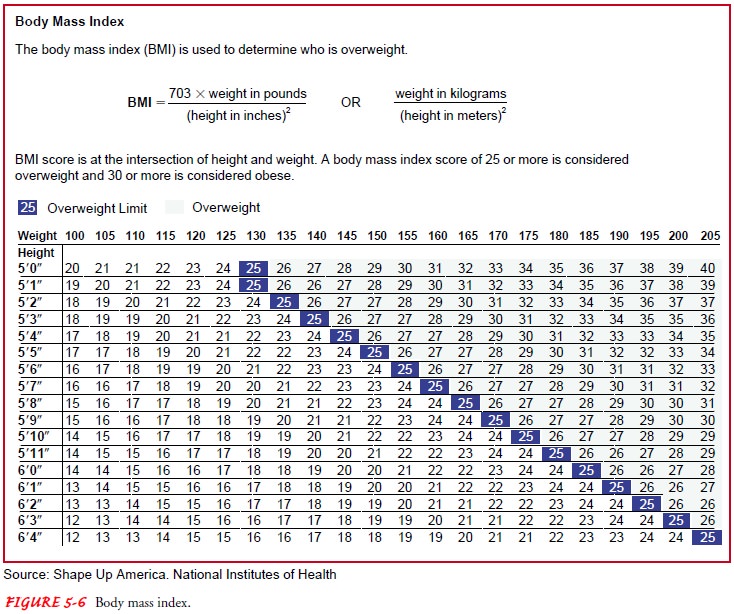
Those who have a BMI of
25 to 29 are considered overweight; those with a BMI of 30 to 39 are considered
obese; above 40 is considered extreme obesity (National Institutes of Health,
2000).
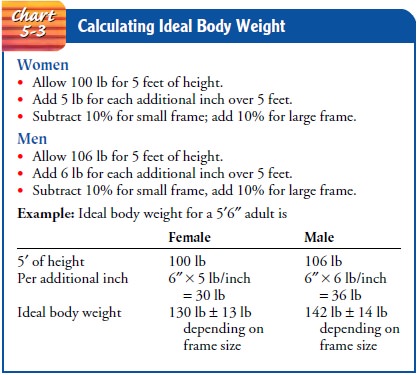
It is important to assess for usual body weight and height. Current weight does not provide information about recent changes in weight; therefore, the patient is asked about his or her usual body weight (Chart 5-3). Decreased height may be due to osteoporosis, an important problem related to nutrition, espe-cially in postmenopausal women. A loss of 2 or 3 inches of height may indicate osteoporosis.
In addition to the calculation of BMI, waist circumference measurement is particularly useful for patients who are catego rized as of normal weight or overweight. To measure waist cir-cumference, a tape measure is placed in a horizontal plane around the abdomen at the level of the iliac crest. Men who have waist circumferences greater than 40 inches and women who have waist circumferences greater than 35 inches have excess abdominal fat. Those with a high waist circumference are at increased risk of di-abetes, dyslipidemias, hypertension, and cardiovascular disease (National Institutes of Health, 2000).
BIOCHEMICAL ASSESSMENT
Biochemical assessment
reflects both the tissue level of a given nu-trient and any abnormality of
metabolism in the utilization of nu-trients. These determinations are made from
studies of serum (serum protein, serum albumin and globulin, transferrin,
retinol-binding protein, hemoglobin, serum vitamin A, carotene, and vi-tamin C)
and studies of urine (creatinine, thiamine, riboflavin, niacin, and iodine).
Some of these tests, while reflecting recent intake of the elements detected,
can also identify below-normal levels when there are no clinical symptoms of
deficiency (see Table 5-1 for a description of serum protein indices).
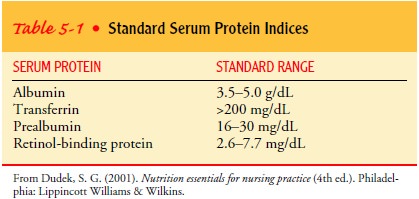
Low serum albumin and
transferrin levels are often used as mea-sures of protein deficits in adults
and are expressed as percentages of normal values. Albumin synthesis depends on
normal liver func-tion and an adequate supply of amino acids. Because the body
stores a large amount of albumin, the serum albumin level may not decrease
until malnutrition is severe; thus, its usefulness in detect-ing recent protein
depletion is limited. Decreased albumin levels may be due to overhydration,
liver or renal disease, and excessive protein loss because of burns, major surgery,
infection, and cancer (Dudek, 2000). Transferrin is a protein that binds and
carries iron from the intestine through the serum. Because of its short
half-life, decreased transferrin levels respond more quickly to protein
deple-tion than albumin. Serial measurements of these, as well as preal-bumin
levels, are used to assess the results of nutritional therapy.
Although not available
from many laboratories, retinol-binding protein may be a useful means of
monitoring acute, short-term changes in protein status.
Reduced total lymphocyte
count in people who become acutely malnourished as a result of stress and
low-calorie feeding are associated with impaired cellular immunity (Dudek,
2000). Anergy, the absence of an immune response to injection of small
concentrations of recall antigen under the skin, may also indicate malnutrition
because of delayed antibody synthesis and response.
Serum electrolyte levels
provide information about fluid and electrolyte balance and kidney function.
The creatinine/height index calculated over a 24-hour period assesses the
metabolically active tissue and indicates the degree of protein depletion,
com-paring expected body mass for height and actual body cell mass.
24-hour urine sample is obtained, and the amount of creati-nine is measured and compared to normal ranges based on the patient’s height and gender. Values less than normal may indicate loss of lean body mass and protein malnutrition.
CLINICAL EXAMINATION
The state of nutrition
is often reflected in a person’s appearance. Although the most obvious physical
sign of good nutrition is a normal body weight with respect to height, body
frame, and age, other tissues can serve as indicators of general nutritional
status and adequate intake of specific nutrients; these include the hair, skin,
teeth, gums, mucous membranes, mouth and tongue, skeletal muscles, abdomen,
lower extremities, and thyroid gland (Table 5-2). Specific aspects of clinical
examination useful in identifying nutritional deficits include oral examination
and as-sessment of skin for turgor, edema, elasticity, dryness, subcuta-neous
tone, poorly healing wounds and ulcers, purpura, and bruises. The
musculoskeletal examination also provides informa-tion about muscle wasting and
weakness.

DIETARY DATA
The appraisal of food
intake considers the quantity and quality of the diet and also the frequency
with which certain food items and nutrients are consumed. Commonly used methods
of deter-mining individual eating patterns include the food record and the
24-hour food recall, which can help estimate if the food intake is adequate and
appropriate. If these methods are used, instructions about measurement and
recording food intake are given when the patient’s dietary history is obtained.
Food Record
The food record is used
most often in nutritional status studies. The person is instructed to keep a
record of food actually con-sumed over a period of time, varying from 3 to 7
days, and to ac-curately estimate and describe the specific foods consumed.
Food records are fairly accurate if the person is willing to provide fac-tual
information and able to estimate food quantities.
24-Hour Recall
The 24-hour recall
method is, as the name implies, a recall of food intake over a 24-hour period.
The person is asked by the in-terviewer to recall all food eaten during the
previous day and to estimate the quantities of the food consumed. Because
informa-tion does not always represent usual intake, at the end of the
in-terview the patient is asked if the previous day’s food intake was a typical
one. To obtain supplementary information about the typical diet, the
interviewer also asks how frequently the person eats foods from the major food
groups.
CONDUCTING THE DIETARY INTERVIEW
The success of the interviewer in obtaining information for di-etary assessment depends on effective communication, which re-quires that good rapport be established to promote respect and trust. The interviewer explains the purpose of the interview. It is conducted in a nondirective and exploratory way, allowing the respondent to express feelings and thoughts while encouraging him or her to answer specific questions. The manner in which questions are asked will influence the respondent’s cooperation. Thus, the interviewer must be nonjudgmental and avoid ex-pressing disapproval, either verbally or by facial expression.
Character of General Intake
Several questions may be
necessary to elicit the information needed. When attempting to elicit information
about the type and quan-tity of food eaten at a particular time, the
interviewer avoids lead-ing questions, such as, “Do you use sugar or cream in
your coffee?” Also, assumptions are not made about the size of servings;
instead, questions are phrased so that quantities are more clearly deter-mined.
For example, to help determine the size of one hamburger eaten, the patient may
be asked, “How many servings were pre-pared with the pound of meat you bought?”
Another approach to determining quantities is to use food models of known sizes
in es-timating portions of meat, cake, or pie or to record quantities in common
measurements, such as cups or spoonfuls (or according to the size of
containers, when discussing intake of bottled beverages).
In recording a particular
combination dish, such as a casserole, it is useful to ask for the ingredients
in the recipe, recording the largest quantities first. When recording
quantities of ingredients, one notes whether the food item was raw or cooked
and the number of servings provided by the recipe. When the client lists the
foods for the recall questionnaire, it may be helpful to read back the list of
foods and ask if anything was forgotten, such as fruit, cake, candy,
between-meal snacks, or alcoholic beverages.
Additional information
obtained during the interview should include methods of preparing food, sources
available for food (donated foods, food stamps), food-buying practices, vitamin
and mineral supplements, and income range.
Cultural and Religious Considerations
An individual’s culture
determines to a large extent which foods are eaten and how they are prepared
and served. Culture and reli-gious practices together often determine if
certain foods are pro-hibited and if certain foods and spices are eaten on certain
holidays or at specific family gatherings. Because of the importance of culture
and religious beliefs to many individuals, it is important to be sensitive to
these factors when obtaining a dietary history. It is, however, equally
important not to stereotype individuals and assume that because they are from a
certain culture or religious group, they adhere to specific dietary customs.
Culturally sensitive
materials, such as the food pagoda, are available for making appropriate
dietary recommendations (The Chinese Nutrition Society, 1999).
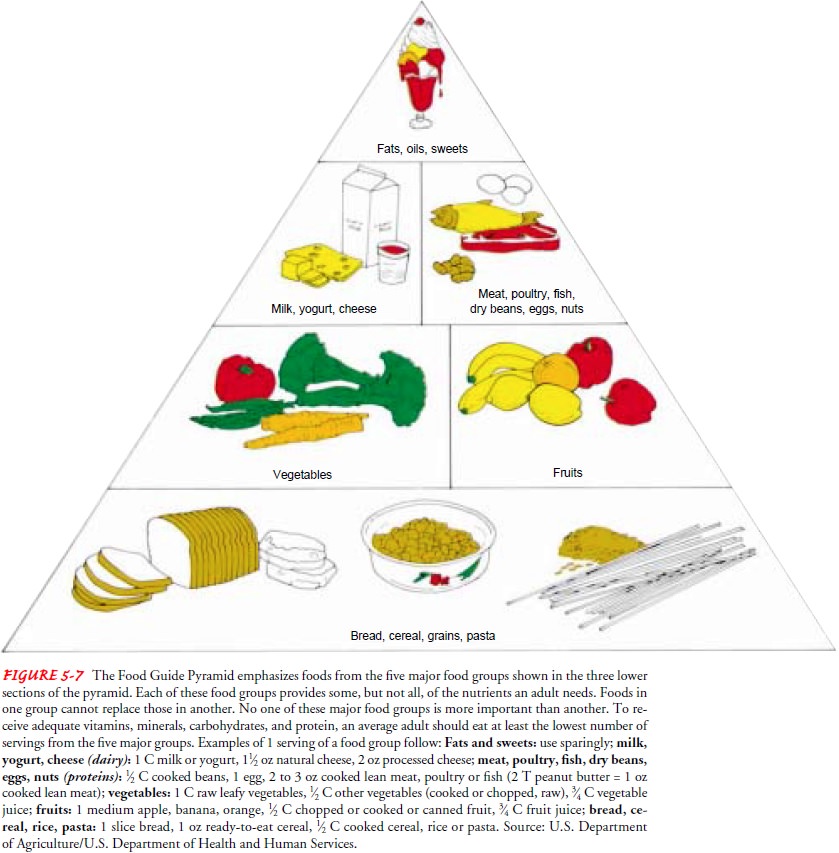
EVALUATING THE DIETARY INFORMATION
After the dietary
information has been obtained, the nurse evalu-ates the patient’s dietary
intake. If the goal is to determine if the per-son generally eats a healthful
diet, the food intake may be compared to the dietary guidelines outlined in the
USDA’s Food Guide Pyra-mid (Fig. 5-7). The pyramid divides foods into five
major groups and offers recommendations for variety in the diet, proportion of
food from each food group, and moderation in eating fats, oils, and sweets. The
person’s food intake is compared with recommenda-tions based on various food
groups for various age levels.
If the nurse or
dietitian is interested in knowing about the in-take of specific nutrients,
such as vitamin A, iron, or calcium, the patient’s food intake is analyzed by
consulting a list of foods and their composition and nutrient content. The diet
is then analyzed in terms of grams and milligrams of specific nutrients. The
total nutritive value is then compared with the recommended dietary allowances
that are specific for different age categories, gender, and special
circumstances such as pregnancy or lactation (Monsen, 2000). The nurse
frequently participates in the nutrition screen-ing of patients and
communicates the information to the dieti-tian and the rest of the team for
more detailed assessment and for clinical nutrition intervention.
FACTORS INFLUENCING NUTRITIONAL STATUS IN VARIED SITUATIONS
One sensitive indicator
of the body’s gain or loss of protein is its nitrogen balance. An adult is said
to be in nitrogen equilibrium when the nitrogen intake (from food) equals the
nitrogen output
A positive nitrogen balance exists when
nitrogen intake exceeds nitrogen output and indicates tissue growth, such as
occurs during preg-nancy, childhood, recovery from surgery, and rebuilding of
wasted tissue. Negative nitrogen balance indicates that tissue is breaking down
faster than it is being replaced. In the absence of an adequate intake of
protein, the body converts protein to glucose for energy. This can occur with
fever, starvation, surgery, burns, and debili-tating diseases. Each gram of
nitrogen loss in excess of intake rep-resents the depletion of 6.25 g of
protein or 25 g of muscle tissue. Therefore, a negative nitrogen balance of 10
g/day for 10 days could mean the wasting of 2.5 kg (5.5 lb) of muscle tissue as
it is converted to glucose for energy.
When conditions that
result in negative nitrogen balance are coupled with anorexia (loss of
appetite), they can lead to malnutrition. Malnutrition interferes with wound
healing, in-creases susceptibility to infection, and contributes to an
in-creased incidence of complications, longer hospital stay, and prolonged
confinement of the patient to bed (Bender, Pusateri, Cook et al., 2000).
The patient who is
hospitalized may have an inadequate di-etary intake because of the illness or
disorder that necessitated the hospital stay or because the hospital’s food is
unfamiliar or unap-pealing (Dudek, 2000; Wilkes, 2000). The person who is cared
for at home may feel too sick or fatigued to shop and prepare food or may be
unable to eat because of other physical problems or limitations. Limited or
fixed incomes or the high costs of med-ications may result in insufficient
money to buy nutritious foods. Patients with inadequate housing or inadequate
cooking facilities are unlikely to have an adequate nutritional intake.
Because complex
treatments (eg, ventilators, intravenous in-fusions, chemotherapy) once used
only in the hospital setting are now being provided in the home and outpatient
settings, nutri-tional assessment of the patient in these settings is an
important aspect of home and community-based care as well as hospital-based
care (Dabrowski & Rombeau, 2000; Worthington, Gilbert & Wagner, 2000).
Many medications
influence nutritional status by suppress-ing the appetite, irritating the
mucosa, or causing nausea and vomiting. Others may influence bacterial flora in
the intestine or directly affect nutrient absorption so that secondary
mal-nutrition results. People who must take many medications in a single day
often report feeling too full to eat. The person’s use of prescription and
over-the-counter medications and their ef-fect on appetite and dietary intake
are assessed. Many of the fac-tors that contribute to poor nutritional status
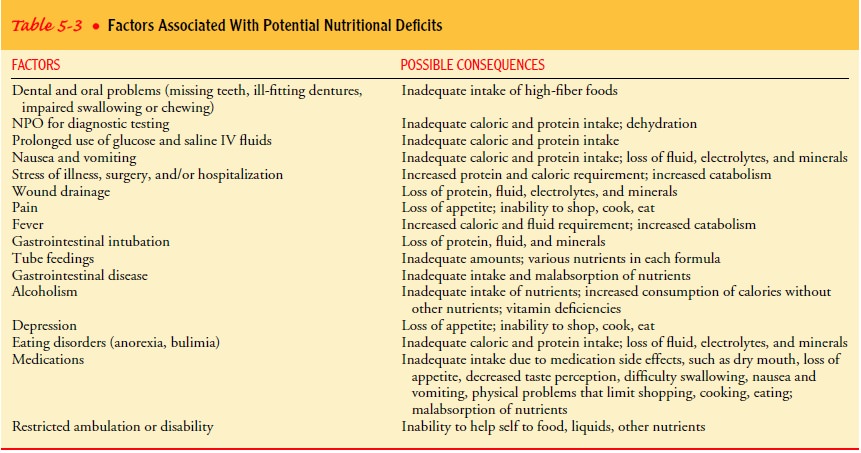
are identified in Table 5-3.
ANALYSIS OF NUTRITIONAL STATUS
Measurement of BMI and
biochemical, clinical, and dietary data are used together to determine the
patient’s nutritional status. Often the BMI, biochemical measures, and dietary
data provide more information about the patient’s nutritional status than the
clinical examination; the clinical examination may not detect subclinical
deficiencies unless such deficiencies become so ad-vanced that overt signs
develop. A low intake of nutrients over a period of time may lead to low
biochemical levels and without nutritional intervention may result in
characteristic and observ-able signs and symptoms (see Table 5-2). A plan of
action for nu-tritional intervention is based on the results of the dietary
assessment and the patient’s profile. To be effective, the plan must meet the
patient’s need for a balanced diet, maintain or con-trol weight, and compensate
for increased nutritional needs.
Adolescent
Considerations
Adolescence is a time of
critical growth and acquisition of lifelong eating habits, and therefore
nutritional assessment and analysis are critical. In the past two decades the
percentage of adolescents who are overweight has almost tripled (USDHHS, 2001).
De-spite this, total milk consumption has decreased by 36% com-pared to prior
years (Cavadini, Siega-Riz & Popkin, 2000). Fruit and vegetable consumption
is also below the recommended five servings per day.
Adolescent girls are at
particular nutritional risk as iron, folate, and calcium intake is below
recommended levels (Cavadini, Siega-Riz & Popkin, 2000). Persons with other
nutritional disorders, such as anorexia and bulimia, have a better chance for
recovery if these disorders are identified in the adolescent years compared to
adulthood (Orbanic, 2001).
Related Topics