Chapter: Surgical Pathology Dissection : The Urinary Tract and Male Genital System
Testis : Surgical Pathology Dissection
Testis
Biopsies
The most
important thing to remember when processing a testicular biopsy is to treat it
gently. The delicate sponge-like consistency of the testic-ular parenchyma
makes it particularly suscepti-ble to desiccation and compression. Be sure that
the tissue remains in fixative during transporta-tion and processing. Bouin’s
solution is a better fixative for these biopsies than is formalin. Take care
not to crush the tissue when transferring the specimen to the tissue cassette.
Do not use forceps; instead, gently filter the specimen into tissue paper. The
entire specimen should be em-bedded and sectioned at multiple levels.
Radical Orchiectomies
When the
entire testis is resected, it is usually removed in continuity with the epididymis
and a variable length of the spermatic cord. Orchiec-tomy specimens can be
oriented with relative ease using the epididymis as a landmark. The epididymis
is roughly a C-shaped structure that cups the testis along its posterior
aspect. Between the posterior aspect of the testis and epididymis is the
mediastinum testis, where ducts, nerves, and vessels enter and exit the testis.
The rete testis is a network formed in the mediastinum testis by the
seminiferous tubules. Always be aware of the location of the mediastinum during
your dissection because neoplasms and infections may extend beyond or into the
testis at this site.
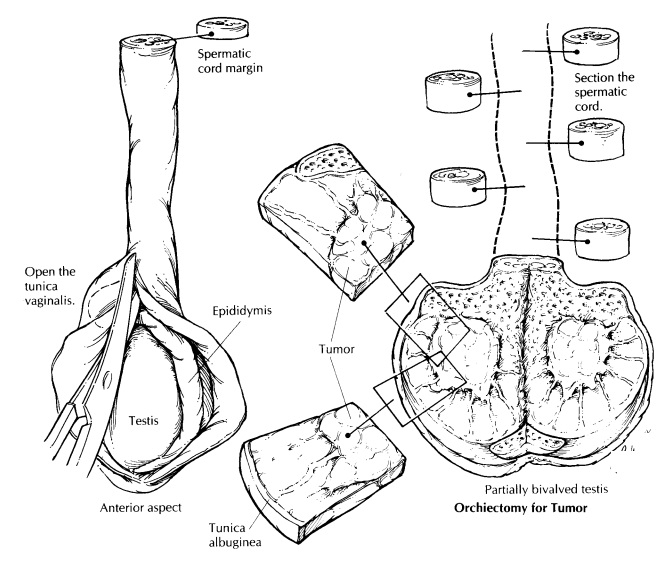
After
the specimen has been oriented and all the structures attached to the testis
have been identified, weigh and measure the testis andepididymis, and record
the dimensions of the spermatic cord. The tunica vaginalis is a thin membranous
sac that covers the external surface of the testis. After noting the appearance
of its outer surface, open the tunica vaginalis along the anterior surface of
the testis. Record the volume and appearance of any fluid that may have
accumulated within this space, and examine the inner surface of the tunica for
thickening or exophytic growths. Due to the noncohesive nature of germ cell
tumors, it is a good idea to obtain sections of the spermatic cord before
in-cising the main tumor to avoid contamination. Shave the spermatic cord
margin and also submit cross sections from each of the three levels of the
spermatic cord (proximal, mid, and distal).
The
tunica albuginea is the thick fibrous cap-sule of the testis. Keep in mind that
this resilient covering makes for an effective barrier to the dif-fusion of
formalin and an equally formidable bar-rier to a dull knife. The testis should
therefore be sectioned with a sharp knife before it is placed in fixative. As
illustrated, partially bisect the testis along its long axis. Begin the cut
along the ante-rior surface (the side opposite the epididymis), and extend the
section into the mediastinum testis. The testis can now be opened much like a
book, with the epididymis serving as the book-binding. This initial section
will optimize your ability to assess the relationship between any focal lesions
and the testicular parenchyma, the tunica albuginea, and the epididymis. Further-more,
this section will allow formalin to penetrate and fix the testicular
parenchyma. After making the initial section, photograph the specimen and
collect tissue for special studies as indicated. A frozen section or touch
preparation from the surface of the lesion may be used to determineif tissue
needs to be sent for microbiologic stud-ies, for a lymphoma workup, or for
electron microscopy.
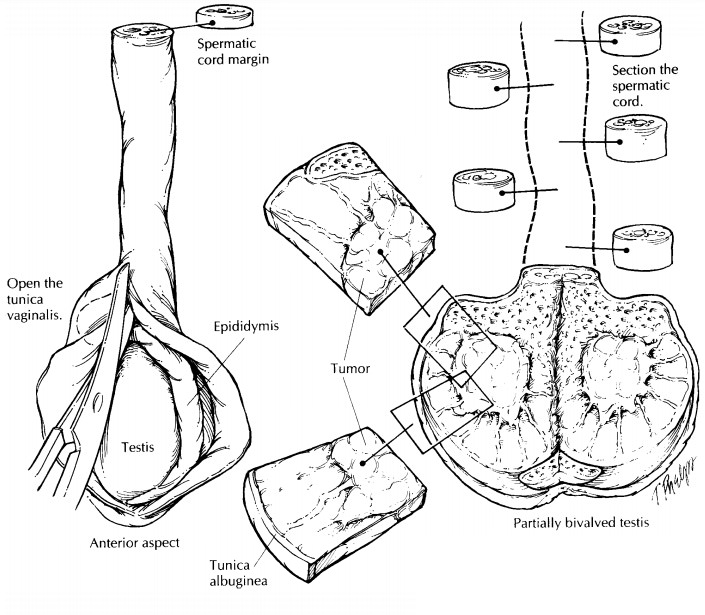
After
the specimen is well fixed, it can be thinly sectioned at 3-mm intervals.
Bread-loaf the testis along its long axis parallel to the initial section. The
epididymis should be sectioned from its head to its tail at right angles to its
long axis. As illustrated, this is best accomplished from the posterior aspect
of the specimen. If you have not already done so, serially section the
remain-ing cord at regular intervals along its entire length.
Carefully
examine the cut surface of the testis and paratesticular tissues. Give a
detailed de-scription of the appearance of any lesions, and try to determine
their location in the testis or paratestis (e.g., central, inferior pole,
superior pole, testicular hilum, epididymis, paratesticu-lar soft tissue,
spermatic cord). When describing the appearance of a testicular mass, be sure
to note its size and areas of hemorrhage and/or necrosis, even if these areas
appear small and inconsequential. Try to determine if the tumor is confined to
the testicular parenchyma, or if there is extratesticular extension, either
beyond the tunica albuginea or into the epididymis. If a testicular neoplasm is
clinically suspected, but one cannot be found on gross inspection, do not give
up. Instead, scrupulously inspect the thin sections for any scars or areas of
gritty calci-fication. These findings may represent regressive changes in a pre-existing
neoplasm.
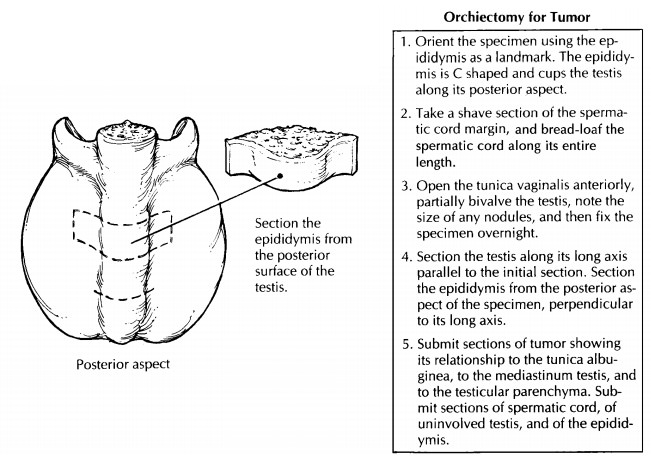
The
standard sections to be submitted from any orchiectomy specimen include: (1)
sections of tumor showing its relationship to the tunica albuginea and to the
mediastinum testis; (2) sec-tions of the testicular parenchyma; (3) sections of
the epididymis; (4) sections of the spermatic cord margin; and (5) sections
from three levels of the spermatic cord (i.e., proximal, mid, and distal). The
number of sections that should be submitted is highly dependent on the clinical
setting. Some of the more common reasons for which the testis is resected are
cited below, along with some guidelines to keep in mind when sampling these
specimens.
Sampling Testicular Neoplasms
Primary
testicular neoplasms often exhibit more than one morphologic component (e.g.,
seminoma and embryonal carcinoma). Because even the focal presence of an
aggressive component may affect the treatment and prognosis, it is critical
that all of the components present be demon-strated histologically. When
submitting sections of primary testicular neoplasms, aim to be both thorough
and selective. To be thorough, submit at least one section of tumor for every 1
cm of its greatest diameter. To be selective, sample the areas of the tumor
that appear distinct on gross examination. For example, be sure to submit
sections from areas of hemorrhage, necrosis, or mucinous change, even if these
areas represent only a minor component of the tumor’s gross appearance. These
gross changes often correlate with important histologic features.
![]()
Sometimes
a primary testicular tumor can re-gress, leaving only a small scar. When a
tumor cannot be identified in a testis removed from a patient with a metastatic
germ cell tumor, the testis should be entirely submitted for micro-scopic
examination.
Undescended Testis
The
undescended testis is vulnerable to torsion, infarction, and most importantly,
the develop-ment of germ cell neoplasms. Thus, a testis that is maldescended is
often resected even when a tumor is not clinically apparent. Your principal
role in the processing of the undescended testis is to determine if a neoplasm
is present. Because early neoplastic changes or regressed tumors may not be
apparent on gross examination, sample generously all areas of the testis even
when a focal lesion is not seen. Just as in the normally positioned testis, an
undescended testis removed from a patient with a metastatic germ cell tumor
should be entirely submitted if a testicular tumor is not grossly apparent.
Bilateral Orchiectomies for Prostate Cancer
The
testes removed from patients with metastatic prostatic carcinoma are not
necessarily abnormal. Instead, bilateral orchiectomies in these patients are
usually done as a therapeutic procedure to remove a source of testosterone.
Nonetheless, carefully examine the specimen for a metastasis or an unsuspected
primary tumor. If none is found,submit one section of the testicular parenchyma
from each testis.
Torsion, Infarction, and Infectious Disease
For
infectious processes, infarcts, and torsion, be sure to submit sections from
both the periphery and the center of any lesions. The duration of testicular
torsion and the host response to an in-fectious agent are best evaluated in the
viable tissue at the periphery of a lesion. Also, when dealing with
inflammatory lesions of the testis, always remember to submit fresh tissue for
microbiologic studies.
Anorchia and Intersex Syndromes
Sometimes
the pathologist is called on to deter-mine the presence and/or type of gonadal
tis-sue in a surgical specimen. In these instances, it is of critical
importance that the specimen be reviewed and oriented with the surgeon. Label
all of the grossly identifiable structures, and photograph the specimen so that
the histologic findings can be correlated with the structures identified
grossly. Always submit a section for histologic evaluation of each structure
identifiedgrossly. When the testis cannot be grossly iden-tified, submit the
entire tissue so that it can be evaluated for histologic evidence of testicular
regression.
Important Issues to Addressin Your Surgical Pathology Report on Orchiectomies
· What
procedure was performed, and what structures/organs are present?
· Is a
neoplasm present?
· Where
does the tumor originate (i.e., testis, epididymis, spermatic cord)?
· What is
the size of the tumor?
· What are
the histologic type and grade of the neoplasm? Is intratubular germ cell
neoplasia present?
· Is the
tumor limited to the testis? Does the tumor extend into any of the adjacent
struc-tures: rete testis, epididymis, spermatic cord, tunica albuginea, or
scrotum?
· Can
vascular invasion be identified histolog-ically?
· If a
neoplasm cannot be identified, is there histologic evidence of intratubular
germ cell neoplasia, calcification, or scar formation?
· Does the
tumor involve any of the margins?
Related Topics