Chapter: Surgical Pathology Dissection : The Urinary Tract and Male Genital System
Prostate : Surgical Pathology Dissection
Prostate
Biopsies
Needle
biopsies of the prostate consist of delicate and thin cores of tan soft tissue.
Measure each piece of tissue, and document the total number of pieces before
carefully transferring them into a tissue cassette. As is true for any small
biopsy, do not use forceps to pick up these biopsies, because forceps can squeeze
and distort the tissue. Have the histology laboratory section these biopsies at
multiple levels, then have them stain alternating levels for routine histology.
If sections are later needed for additional studies (e.g., immunoperoxidase),
the unstained slides will be readily available, and diagnostic material will
not be lost during sectioning of the tissue block.
Transurethral Resections and Open Enucleations
Frequently,
the central region of the prostate is removed—either by transurethral resection
or by open enucleation—to relieve symptoms of uri-nary obstruction caused by
nodules compressing the prostatic urethra. Although the majority of these
nodules are entirely benign, a small, yet significant percentage (i.e., 10%)
harbor a carci-noma.
Tissue
fragments obtained from transurethral resections of the prostate—referred to as
prostatechips—are generally tan,
rubbery, and cylindrical.The total number of chips resected varies greatly from
case to case. Measure the combined weightof the chips, and record their
aggregate dimen-sions. For larger specimens, it is not practical to submit all
of the chips for histologic evaluation. Although six to eight tissue cassettes
are gener-ally sufficient to detect the vast majority of inci-dental
carcinomas, the sensitivity of sampling can be increased by selectively
submitting those chips that appear yellow, indurated, or in any other way
grossly suspicious for carcinoma. More extensive sampling is warranted in
specimens from younger patients, since even a small focus of carcinoma in these
men may require aggressive therapy. For patients under the age of 65, consider
submitting the entire specimen for histologic evaluation. Similarly, if cancer
is identified histo-logically in a specimen that was partially submit-ted, the
entire specimen should be submitted so that the approximate volume of the
cancer can be calculated.
Specimens
obtained by open enucleation are either partially or totally intact nodules,
but the anatomic orientation of these nodules is usually not practical or
possible. After weighing and mea-suring the tissue, serially section the
specimen at 2- to 3-mm intervals. Note the appearance of the cut surface.
Again, extensively sample the specimen to detect incidental carcinomas. Submit
up to six to eight cassettes of tissue. As was true for the prostate chips,
remember to selectively sample areas that appear grossly suspicious for
carcinoma.
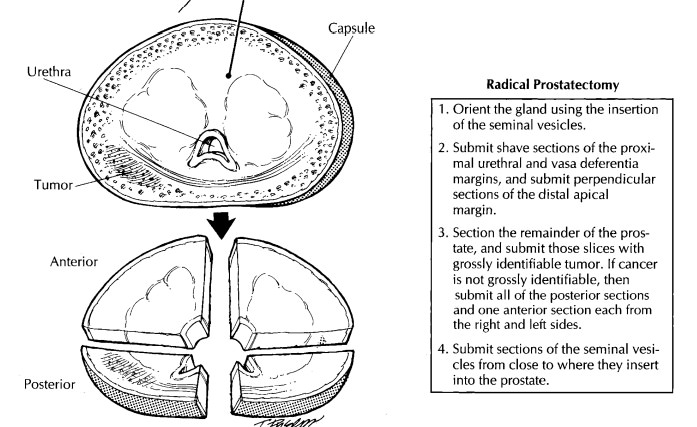
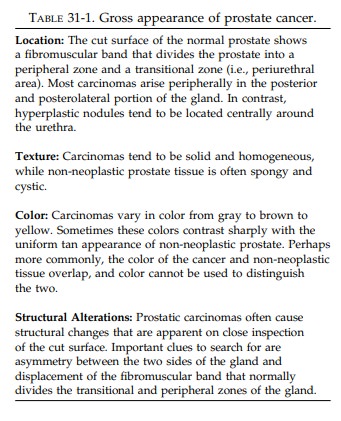
Radical Prostatectomies
One of
the challenges of the dissection of radical prostatectomies is to find a
balance which willmaximize prognostic information while mini-mizing the number
of tissue cassettes submitted. Selective sampling of a carcinoma of the
prostate can be difficult because subtle differences in the gross appearance of
cancer and non-neo-plastic prostate tissue can be hard to recognize. This is
why it is so important that you familiarize yourself with the subtleties of the
gross appearance of prostate cancer. A number of the gross features of prostate
cancer are outlined in Table 31-1 and can be helpful in distinguishing
carcinoma from non-neoplastic tissue.
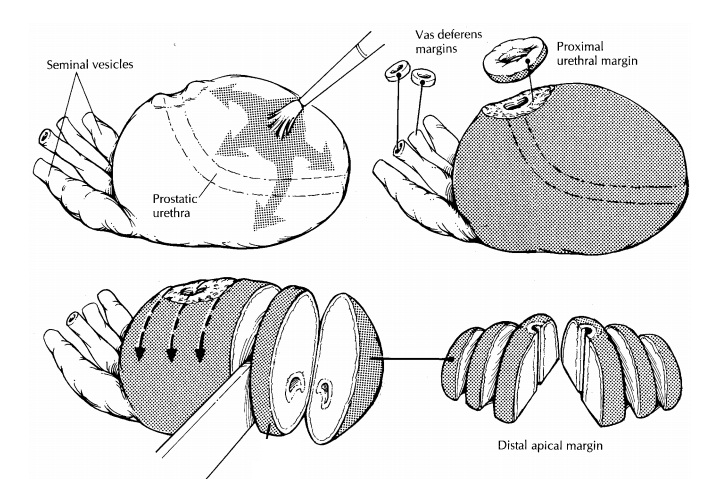
Orient the prostate by locating the seminal vesi-cles and vasa deferentia. These structures insert into the posterior aspect of the base (proximal end) of the gland and provide a landmark that is quick and easy to find. In contrast to the broad and flat base, the apex (distal end) of the prostate narrows and becomes cone shaped. The contour of the gland can be used to distinguish the anterior and posterior aspects of the prostate. The anterior sur-face of the prostate is rounded and convex, while the posterior surface is broad and flat. After orient-ing the specimen, weigh and measure it. Inspect the intact prostate for asymmetry, and palpate it for areas of induration. Paint the surfaces of the pros-tate with ink. Fixation of the prostate before sec-tioning permits thinner sectioning of the gland and better assessment of the margins.
Relatively recent
fixation protocols that utilize microwave fixation, such as that described by
Ruijter and coworkers,16 have significantly reduced
fixation times. Indeed, radical prostatectomy specimens can now be fixed and
sectioned on the same day as the surgery.![]()
Following
fixation, thinly shave the vasa defer-entia and the proximal (bladder neck)
margins. The distal (apical) margin can be submitted in one of two ways. One
method is to submit this margin as a thinly shaved section. A second method is
illustrated. Amputate the distal 1 cm of the apex, then section this apical cone
at right angles to the cut edge in thin parallel slices. The latter tech-nique
allows for a more accurate assessment of exactly how close the cancer
approaches the distal (apical) margin. If the proximal (bladder neck) and
distal (apical) margins are taken as shave sections, these sections should be
very thin (1 mm in thickness). A common misunderstanding among pathologists is
that these sections are taken to assess the status of the prostatic urethral
margins. They are not. These sections are taken to sample the bladder neck
margin. Once transected during surgery, the urethra retracts into the gland.
Thus there is no need to obtain urothelium on these margin sections, and you
should avoid the tendency to submit thick doughnut-shaped sections with urothelium
in the center. The semi-nal vesicles are evaluated by taking a section through
the base of the seminal vesicle where it joins the prostate. It is not
necessary to submit entire tips of the seminal vesicles.
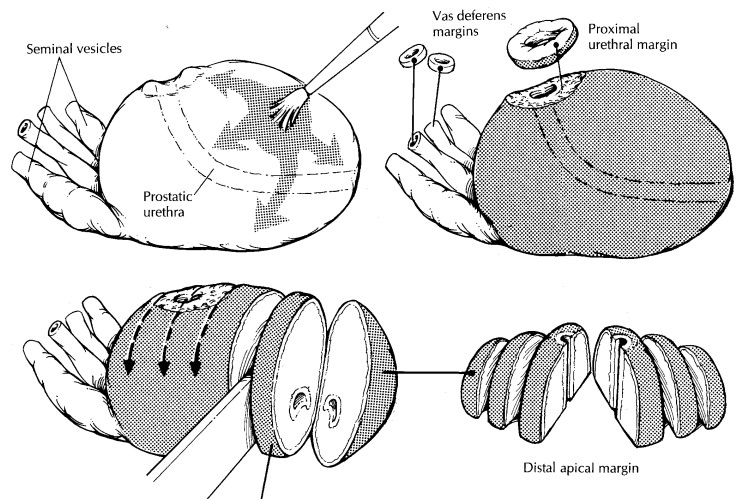
After
the margins have been taken, serially sec-tion the prostate at 2- to 3-mm
intervals from apex to base. Do not use the urethra as a point of reference for
these sections, because this structure follows a curved course through the
prostate. In-stead, section the prostate perpendicular to the broad flat
posterior surface of the gland. The carefully sectioned prostate can be likened
to a loaf of sliced bread. Each individual slice should be intact, uniformly
thin, and surrounded by a ‘‘crust’’ of prostatic capsule and inked soft tissue.
You will come to realize the importance of this crust when you later have to
evaluate the histo-logic sections for extraprostatic extension of the tumor.
Lay the
individual slices out sequentially from apex (distal) to base (proximal). Be
careful to maintain the orientation (i.e., right vs. left, ante-rior vs.
posterior) of each slice. Beginning at the apex and proceeding to the base,
designateeach slice (e.g., A, B, C). This will enable you to remember the
location of each individual slice within the prostate.
Several
key landmarks guide the examination of the individual slices. The prostatic
urethra is located near the center of each slice. It has a roughly U-shaped
appearance on cut section. The arms of the U point to the posterior surface of
the gland, and its convexity points to the anterior surface. Find the
fibromuscular band of tissue that separates the central/anterior portion of the
gland from the horseshoe-shaped peripheral por-tion of the gland. Try to find
the cancer using the guidelines outlined in Table 31-1. Describe the appearance
of any lesions, carefully noting their location (left or right, anterior or
posterior) and size. Because each slice has already been designated, you can
precisely indicate in your gross description which of the slices appear involved.
The
slices may have to be sectioned further to fit into standard tissue cassettes.
A median sec-tion through the urethra will divide the slice into roughly equal
right and left sides, and a coronal section through the urethra will, when
necessary, further divide the slice into anterior and posterior quadrants.
Although it is common practice in many academic centers to submit the entire
pros-tate for histologic examination, such processing significantly increases
the cost of handling speci-mens and can impose strains on a laboratory’s
resources. As a more efficient alternative, these specimens can be partially
sampled using pro-tocols that vary depending on the presence or absence of
grossly apparent tumor. If you can confidently identify the cancer grossly,
submit slices that contain the entire gross lesion. The question arises as to
how thoroughly to sample the prostate when the tumor is not grossly visi-ble.
We recommend sampling the entire posterior aspect of the prostate along with
one anterior sec-tion from the both the right and left sides of the middle of
the gland. If one of these mid-gland sections shows significant tumor, go back
to the specimen and submit the entire anterior portion of the gland on the side
involved.
After
the specimen has been appropriately sampled, retain the remaining tissue
sections in their original order and orientation in caseadditional sections
must be submitted. One simple method is to fasten the slices together with a
safety pin or rubber band.
Pelvic Lymph Node Dissection
Radical
prostatectomies are usually accompanied by a dissection of the pelvic lymph
nodes. These dissections are generally submitted by the sur-geon as separate
specimens.
Pelvic
lymph node dissections consist of vari-able numbers of lymph nodes embedded in
fibro-fatty connective tissue. Each lymph node should be submitted for
histologic evaluation. Keep in mind that in a small but significant number of
cases the metastatic implants are present in adipose tissues (not in the
grossly recognized lymph nodes). Based on this finding, we submit all adipose
tissue from pelvic lymphadenectomy specimens, at least for cases with biopsy
Gleason scores of 7 or higher.
Important Issues to Address in Your Surgical Pathology Report on Radical Prostatectomies
· What
procedure was performed, and what structures/organs are present?
· Where in
the prostate is the bulk of the tumor located? Does it involve both sides of
the gland?
· What are
the histologic type and grade of the tumor?
· Does the
tumor involve greater than 5% of the tissue resected?
· Does the
tumor extend beyond the prostate (i.e., ‘‘extraprostatic extension’’).
· Is
vascular or perineural invasion identified?
· Does the
tumor infiltrate the seminal vesicles?
· Is the
tumor present at any of the following margins: proximal (bladder neck) margin,
distal (apical) margin, vasa deferentia margins, or soft tissue margins?
·
Has the tumor metastasized to regional lymph
nodes or pelvic adipose tissue? Record the number of metastases and the total
number of lymph nodes examined.
Related Topics