Chapter: Surgical Pathology Dissection : The Urinary Tract and Male Genital System
Bladder : Surgical Pathology Dissection
Bladder
Biopsies
Biopsy
specimens of the urinary bladder are generally removed through the cystoscope.
They vary from single and minute to numerous, large, and papillary. Orientation
of these specimens is generally impossible, even for the larger papillary
fragments. Biopsies of neoplasms potentially hold important information
regarding tumor type, tumor grade, and extent of tumor invasion into the
various layers of the bladder wall.
By
following two simple rules, you can avoid missing this crucial information.
First, be sure to submit all of the pieces of tissue for processing and
multiple sectioning. Second, avoid the common mistake of overfilling specimen
cassettes with tissue fragments. Keep in mind that portions of the specimen
will not be sampled if they are ‘‘buried’’ within a crowded cassette. In
addition, we strongly recommend that the urologist submit superficial and deep
tumor biopsies as separate specimens to facilitate the detection of deep muscle
invasion.
Total Cystectomies
The
processing of resected urinary bladders can be accomplished in three steps: (1)
orientation of the specimen and identification of relevant structures (e.g.,
ureters); (2) fixation of the specimen; and (3) dissection of the specimen.
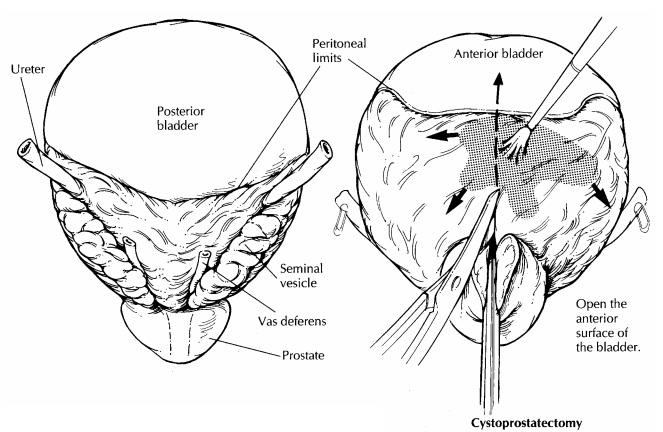
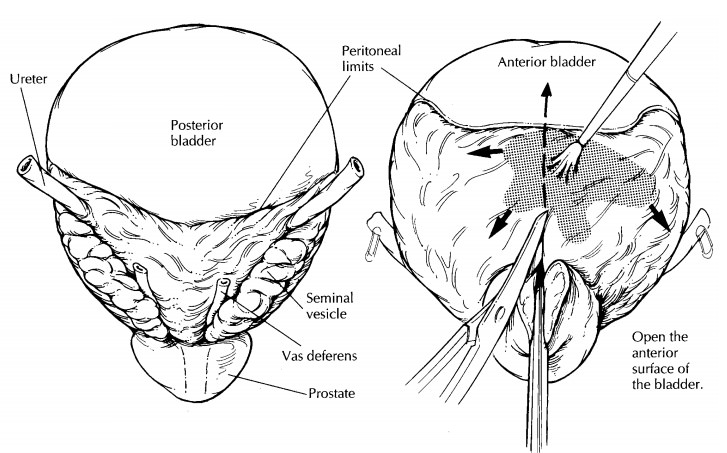
Given the almost spherical shape of the bladder, this first step, orientation,
is not necessarily an easy one. The peritoneum covering the surface of the
bladder can be used as a reliable, though subtle, anatomic landmark. As
illustrated, the peritoneum descends further along the posterior wall of the
bladder than it does along the anterior wall. If they are present, other pelvic
organs can also be used to orient the specimen. For example, the seminal
vesicles and uterus mark the posterior aspect of the bladder. Once the specimen
is oriented, locate both ureters and, when present, the vasa deferentia. The
best place to look for the ureters is in the lateral perivesicular fatty
connective tissues. The ureters are much easier to locate and dissect in the
fresh state than they are once the specimen is fixed. Tag the end of each ureter
with a safety pin so that you can locate them later. The next step is to fix the specimen. Some
prefer to fix bladders in distention, either through the urethra via a catheter
or through the bladder wall using a large-gauge needle. The method we prefer and
describe below is to open the bladder and pin it out before submerging it in
formalin. The advantage of this latter method is that by exposing the tumor
before fixation samples can be collected for ancillary studies requiring fresh
tissue. Begin by inking the surface of the perivesicular soft tissues, and then
open the anterior bladder wall from the urethra to the bladder dome using
scissors. Avoid disrupting the posterior wall, because the ureteral orifices
are located in this region, and they will serve as important anatomic landmarks
later in the dissection. Examine the mucosa for ulcerations, exophytic tumors,
or more subtle mucosal alterations. Note the size, gross morphology (flat,
papillary, or ulcerated), and location (e.g., dome, trigone, free walls) of any
lesions in the bladder. Photograph the opened specimen. Collect fresh tissue
for special studies if warranted. Pin the specimen to a wax block such that the
bladder cavity is opened and the luminal surface is fully exposed, and submerge
the entire specimen in formalin.
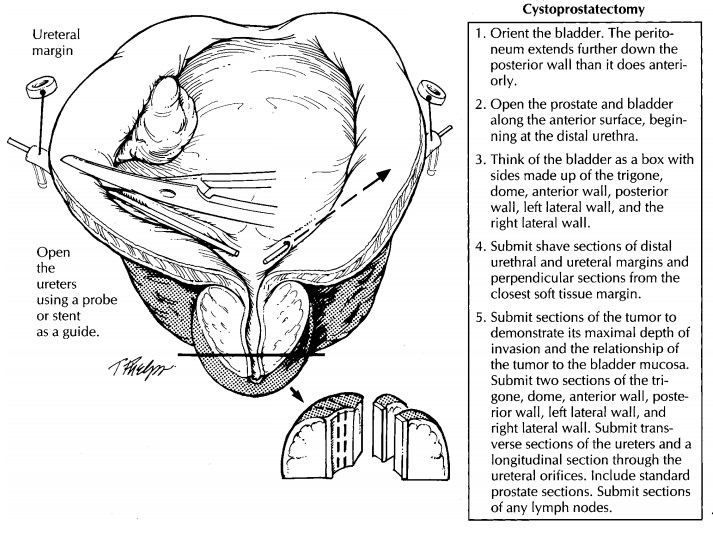
After
the specimen is well fixed, resume the dissection by shaving the margins from
each of the ureters and (when present) the vasa deferen-tia. These already
should have been located and tagged in the fresh specimen. The urethral margin
should also be taken as a thin shave sec-tion. When the specimen includes the
prostate, amputate the distal 1 cm of the prostate at its apex; then section
this apical cone at right angles to the cut edge in thin, parallel sections.
These sections will include the distal portion of the prostatic urethra, and
will permit you to determine precisely the status of the distal margin at the
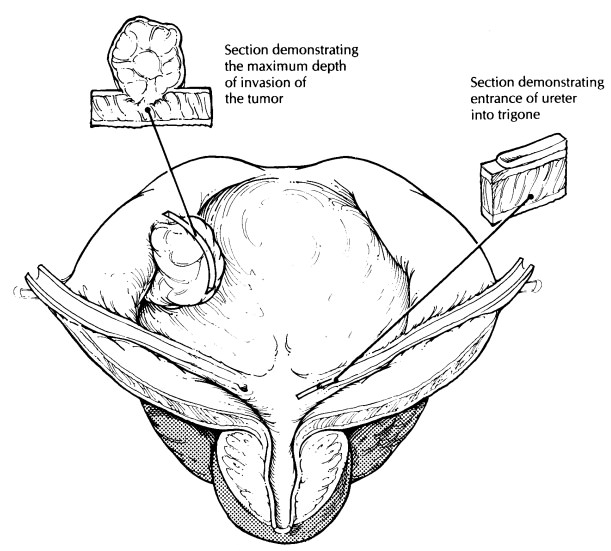
prostatic apex. Next, using a small pair of scissors, open the ureters on both
sides, beginning at their trigone orifices. Look for ureteral strictures and
dilatations, and examine the mucosa for ulcerations or exophytic lesions.
Document these findings in the gross dictation. Submit transverse sections of
the ureters at regular intervals along their entire length.
If a
tumor is identified in the bladder, try to determine its depth of invasion. To
do this, make a full-thickness cut through the tumor and blad-der wall. See
whether the tumor appears to in-filtrate the muscularis propria of the bladder
and, if so, whether it extends into the surrounding soft tissues. Take sections
of the tumor to demon-strate its relationship to the adjacent urothelium and,
importantly, its maximal depth of invasion. Keep in mind that for large
exophytic tumors sections will be more informative when they are taken from the
base of the tumor than when they are taken from its surface.
Urothelial
neoplasms often arise in a back-ground of widespread epithelial alterations.
Fur-thermore, many urothelial neoplasms are treated before surgical resection,
and residual tumors may not be grossly apparent. For these reasons, it is
important that bladders resected for urothelial neoplasia be extensively
sampled for histology, even at sites that appear distant from the tumor. As a
guide for sampling, treat the bladder as though it were a box with six walls
including the floor (trigone), roof (dome), right and left lateral walls,
anterior wall, and posterior wall. Submit two sections from each of these, as
well as long-itudinal sections through the ureteral orifices on both sides.
Selectively sample areas where the mucosa appears abnormal. Carefully inspect
the
bladder mucosa because many in situ
neo-plasms of the bladder are flat and are charac-terized by a subtle red
velvety appearance, in contrast to the tan, smooth appearance of nor-mal
mucosa.
Section
through the perivesicular soft tissues, and look for tumor extension beyond the
bladder wall. Submit perpendicular sections from the soft tissue margins. Be
sure to search for lymph nodes, which are sometimes present in the
perivesicular soft tissues. If any are found, measure them indi-vidually, and
submit each for histologic eval-uation.
Partial Cystectomies
Less
frequently, only a portion of the bladder is removed as a sheet-like piece of
tissue. In gen-eral, these partial cystectomies should be fixed and dissected
according to the guidelines given for complete bladder specimens, keeping in
mind that orientation of these specimens may not always be possible. Rather
than a three-dimensional box, the partial cystectomy can be thought of as a
rectangular sheet with four edges. These edges are important, because they
repre-sent the surgical margins of the bladder wall. Ink the edges and assess
these margins for tumor involvement by taking perpendicular sections from all
edges of the rectangle at regular inter-vals. Remember to include mucosa as
well as the wall of the bladder in these sections. Sections should also be
taken to demonstrate the maxi-mum depth of invasion of the tumor.
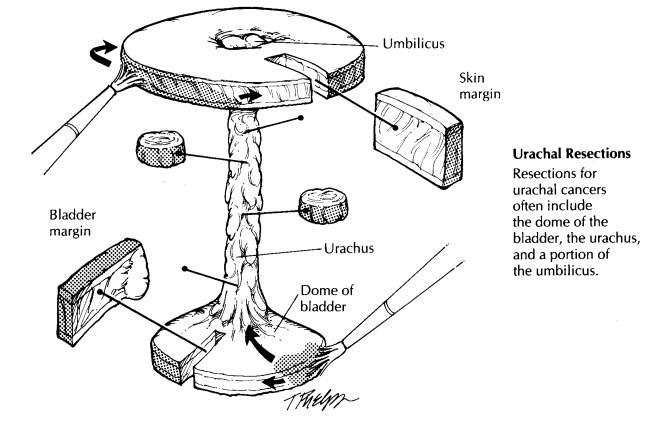
A peculiar variation of the partial cystectomy is seen in resections of neoplasms arising from the urachal tract. These specimens consist of the dome of the bladder in continuity with the ura-chal tract up to and including the umbilicus. As illustrated, the bladder portion of the specimen should be routinely processed as you would any ordinary partial cystectomy. As for the urachal tract, first ink the surrounding soft tissue mar-gins, and then serially section through the tract from the bladder to the umbilicus. These sections should be taken at right angles to the long axis of the urachal tract. Submit a number of these cross sections from the urachal tract for histology as well as the standard bladder sections. Remem-ber to sample the two additional margins intro-duced by this resection: the soft tissue margin surrounding the urachus and the skin margin rimming the umbilicus.
En Bloc Resections
Commonly,
the bladder is removed in continuity with the prostate, uterus, or other pelvic
organs. The added complexity of these specimens intro-duces only minor
alterations to the guidelines given above. For cystoprostatectomies, you will
again need to open the specimen anteriorly before fixing it; only now begin the
incision at the distal prostatic urethra. Using a pair of scissors, open the
prostate anteriorly by cutting along the pros-tatic urethra, and continue the
incision through the anterior bladder wall all the way to the dome. Try not to
disrupt the posterior aspect of the pros-tate with this first longitudinal cut.
After the spec-imen has been opened, carefully examine the urethral mucosa for
evidence of extension of tumor into the prostatic urethra. Once the speci-men
is fixed, serially section the prostate from apex to base at 2- to 3-mm
intervals. These sec-tions should be transverse sections through the posterior
surface of the gland. Examine the cut surface of the prostate. If a tumor is
identified, try to determine if it is arising centrally from the prostatic
urethra or if it is more peripherally located, as is common for cancer of the
prostate. This observation is important, because the pros-tate should be
processed differently
if a
primary prostate carcinoma is present. If no peripheral tumors are noted, then
a more limited sampling of the prostate is in order. These prostate sections
should include (1) shaved margins from the distal vasa deferentia; (2)
per-pendicular sections from the distal (apical) margin of the prostate
including the prostatic urethra; (3) a posterior transverse section from the
apical, mid, and basilar regions of the gland; (4) two cross sections of the
prostatic urethra; and (5) a section of each seminal vesicle.
Because
the other pelvic organs commonly re-moved with the bladder (e.g., uterus and
rectum) are situated posteriorly, use the same anterior approach to open the
bladder without altering its relationship to these other organs. Section these
additional structures, keeping four objectives in mind: (1) document the
presence of these struc-tures; (2) demonstrate the relationship between the
tumor and each of these structures; (3) evalu-ate the resection margins for
each organ; and![]() examine the attached pelvic organs for other
diseases. For example, when a portion of rec-tum accompanies the bladder
specimen, sections should be submitted (1) to document the pres-ence of rectum
and any incidental rectal pathologic findings; (2) to demonstrate the
relationship between the rectum and the tumor; and (3) to assess the status of
the proximal and distal rectal margins.
examine the attached pelvic organs for other
diseases. For example, when a portion of rec-tum accompanies the bladder
specimen, sections should be submitted (1) to document the pres-ence of rectum
and any incidental rectal pathologic findings; (2) to demonstrate the
relationship between the rectum and the tumor; and (3) to assess the status of
the proximal and distal rectal margins.
Important Issues to Address in Your Surgical Pathology Report on Cystectomies
· What
procedure was performed, and what structures/organs are present?
· Is a
neoplasm present?
· Where in
the bladder is the tumor located (tri-gone, anterior wall, posterior wall, left
lateral wall, right lateral wall, dome)?
· How
large is the tumor?
· What is
its pattern of growth? Is it papillary, flat, or ulcerated?
· Is the
neoplasm in situ or infiltrating?
· What are
the size, histologic type, and grade of the neoplasm?
· What is
the maximal depth of invasion of the neoplasm? Does it extend into the lamina
pro-pria, the inner half of the muscularis propria, or the outer half of the
muscularis propria?
· Does the
tumor extend beyond the bladder into the perivesicular fat, prostate, uterus,
vagina, pelvic wall, or abdominal wall?
· For
bladder carcinomas involving the prostate, specify the nature of prostatic
involvement. Specifically, does the carcinoma directly invade the prostate at
the bladder neck? Does the car-cinoma involve the prostatic urethra? Is there
involvement of prostatic ducts with or without stromal invasion?
· What is
the status of each of the margins (the ureters, urethra, soft tissue, etc.)?
· Is the
tumor multifocal or unifocal? Does the tumor involve blood vessels, nerves, or regional lymph
nodes? How many lymph nodes were examined, and how many harbor a metastasis?
Related Topics