Chapter: Medicine Study Notes : Genetics and Cancer
Symptom Management in Cancer
Symptom Management in Cancer
Pain Management in Cancer
·
Principles of symptom control:
o Evaluation: identify each problem/pain and make sure it‟s managed
o Explanation
o Individualised treatment
o Monitoring progress
o Attention to detail
o Anticipate problems
·
Common problems:
o Physical symptoms: pain, anorexia, nausea, insomnia etc
o Compounded by anger, losses, fear, financial insecurity, anxiety,
isolation, bewildered by treatment. Always consider emotional, intellectual and
spiritual components
·
Causes of pain:
o Destructive/obstructive effects of the cancer
o Debility: pressure sores, constipation
o Due to treatment
·
WHO analgesic ladder:
o Step 1: mild pain. Paracetamol,
aspirin, NSAIDs
o Step 2: moderate pain. Codeine,
Tramadol (not subsidised, plus combination drugs:
§ Paradex (Digesic): dextropropoxyphene plus paracetamol
§ Panadine: codeine plus paracetamol
o Step 3: severe pain:
§ Morphine:
· Actions: analgesia, respiratory depression, drowsiness, vomiting, miosis, convulsions, euphoria or Dysphoria, smooth muscle stimulation (® GI muscle spasm, bilary and renal tract spasm)
· Rapid acting oral: morphine elixir (10 mg 4 hourly) or Sevredol tablet (10 or 20 mg): maximum effect after 2 hours
·
Longer acting: MST (duration 8 –
12 hours) or Kapanol (24 hour slow release)
·
PR: rapid acting suppositories or
MST
·
Parenterally: IM (onset in 10 –
15 minutes, lasts 4 hours), SC, IV
·
Bioavailability: half parenteral
dose over oral
·
Anticipate constipation
·
Signs of morphine overdose: RR
< 12, if RR < 8 then Naloxone
§ Methadone (difficult titrating the dose)
§ Fentanyl: less constipation than morphine, but not subsidised,
transdermal fentanyl patches lasting 72 hours are well suited to patients with
stable pain and low to medium opiod requirements
o Adjuvants at any stage: TCAs, anticonvulsants, steroids, muscle
relaxants, antiarrhythmics
·
Anticipate pain and give regular
analgesia, plus PRN medication for acute-on-chronic pain („breakthrough‟ pain)
·
Enhance coping skills:
o Listen and acknowledge the symptoms
o Explanation, information
o Shared decision making
o Calm supportive environment
o Complementary therapies: relaxation, art therapy, music, OT diversional
therapy
o Spiritual support, counselling
o Treat anxiety, depression
o Support the family
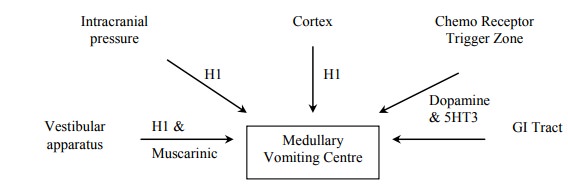
Management of Nausea
·
Identify the right pathway and treat
it specifically:
·
“Drugs of choice”:
o H1 antagonist: cyclizine
o D2 antagonist: Haloperidol
o Prokinetic: Oral domperidone, iv metoclopramide (also has anti-D2
effect)
·
Chemical cause (stimulation of
chemoreceptor trigger zone by uraemia, opioid induced, hypercalcaemia, toxins):
stimulates dopamine receptors. Haloperidol is a dopamine antagonist, as is
chlorpromazine, metoclopramide and cisapride
·
Mechanical cause (squashed
stomach, delayed emptying, regurgitation): Metoclopramide and domperidone ®
prokinetic action
·
Emetogenic chemotherapy:
stimulates release of serotonin in the gut: 5HT3 antagonists are used
(ondansetron, granisetron, tropisetron)
·
Vestibular and ICP: use
antihistamines eg cyclizine
·
Non-drug therapy: prophylactic
treatment of constipation, keep away from sight or small of food; small,
frequent, attractive meals, relaxation therapy, acupressure
Management of Breathlessness
·
Due to effusion, anaemia, mass or
irritant effect, anxiety, fatigue. Compounded by fear of fighting to breath.
Can also be PE (but don‟t anticoagulate them – it‟s better to die from a clot
than a bleed)
·
Low dose morphine ® ¯irritant
respiratory reflexes
·
Anxiolytics for panic (eg
lorazepam for intermittent breathlessness, diazepam for chronic)
·
Steroids for anti-inflammatory
effect
·
Nebulised saline: shift sticky
secretions, humidify dry airways
·
Oxygen if symptomatic hypoxia –
but commits the patient to the equipment
·
Advice from physio, especially re
controlling expiration
·
Fan on face, open window
Management of Cachexia
·
= Marked weight loss and muscle
wasting, especially in advanced GI and lung cancers
·
Due to metabolic
rate and ¯food intake, plus abnormal metabolism and cytokine production
·
May also see altered taste
sensation, loose dentures causing difficulty eating, oedema due to
hypo-albuminaemia, pressure sores over bony prominences, etc
·
Body changes may generate
feelings of fear, isolation or difficulty with relationships
·
Management:
o Dietary supplements and NG feeding are unlikely to achieve anything.
Patients should eat and drink as they wish
o Corticosteroids in a reducing protocol may help (as well as reducing
tumour oedema)
o Relining dentures
o General support: education, new clothes, aides to maintain independence
Related Topics