Chapter: Medical Microbiology: An Introduction to Infectious Diseases: Dermatophytes, Sporothrix, and Other Superficial and Subcutaneous Fungi
Sporotrichosis : Clinical Aspects
SPOROTRICHOSIS : CLINICAL ASPECTS
MANIFESTATIONS
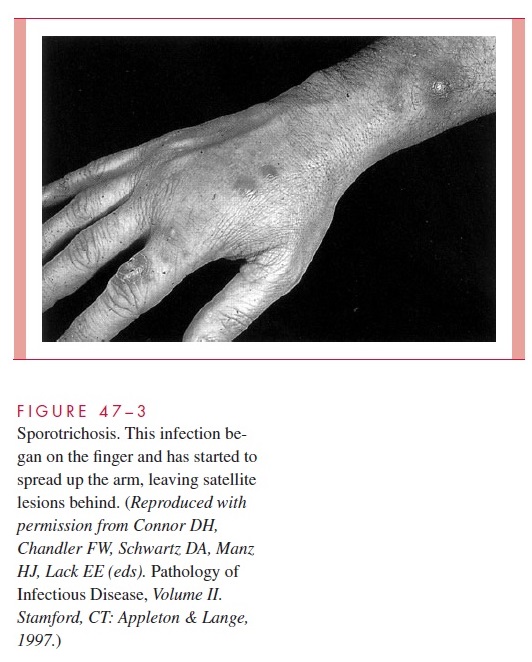
A skin lesion begins as a painless papule that develops a few weeks to a few months after inoculation. Its location can usually be explained by occupational exposure; the hand is most often involved. The papule enlarges slowly and eventually ulcerates, leaving an open sore. Draining lymph channels are usually thickened, and pustular or firm nodular lesions may appear around the primary site of infection or at other sites along the lym-phatic drainage route (Fig 47–3). Once ulcerated, lesions usually become chronic. Multi-ple ulcers often develop if the disease is untreated. Symptoms are those directly related to the local areas of infection. Constitutional signs and symptoms are unusual.
Occasionally, spread occurs by other routes. The bones, eyes, lungs, and central ner-vous system are susceptible to progressive infection if the organisms reach these organs; such spread, however, occurs in less than 1% of all cases. Primary pulmonary sporotri-chosis occurs but is also rare.
DIAGNOSIS
Direct microscopic examination for S. schenckii is usually unrewarding because there are too few organisms to detect readily with potassium hydroxide preparations. Even specially stained biopsy samples and serial sections are usually negative, although the presence of a histopathologic structure, the asteroid body, is suggestive. This structure is composed of S. schenckii yeast cells surrounded by amorphous eosinophilic “rays.” Definitive diagnosisdepends on culture of infected pus or tissue. The organism grows within 2 to 5 days on all media commonly used in medical mycology. Identification requires demonstration of the typical conidia and of dimorphism.
TREATMENT AND PREVENTION
Cutaneous sporotrichosis is effectively treated with a saturated solution potassium iodide (SSKI) administered orally. Systemic infections require the use of amphotericin B and/or azoles. Clinical experience with itraconazole has been excellent, and it may become the treatment of choice for all but cutaneous sporotrichosis. Eradication of the environmental reservoir of S. schenckii is not usually practical, although the mine outbreak mentioned previously was stopped by applying antifungal agents to the mine shaft timbers.
Related Topics