Chapter: Medical Microbiology: An Introduction to Infectious Diseases: Dermatophytes, Sporothrix, and Other Superficial and Subcutaneous Fungi
Dermatophytoses : Clinical Aspects
DERMATOPHYTOSES : CLINICAL ASPECTS
MANIFESTATIONS
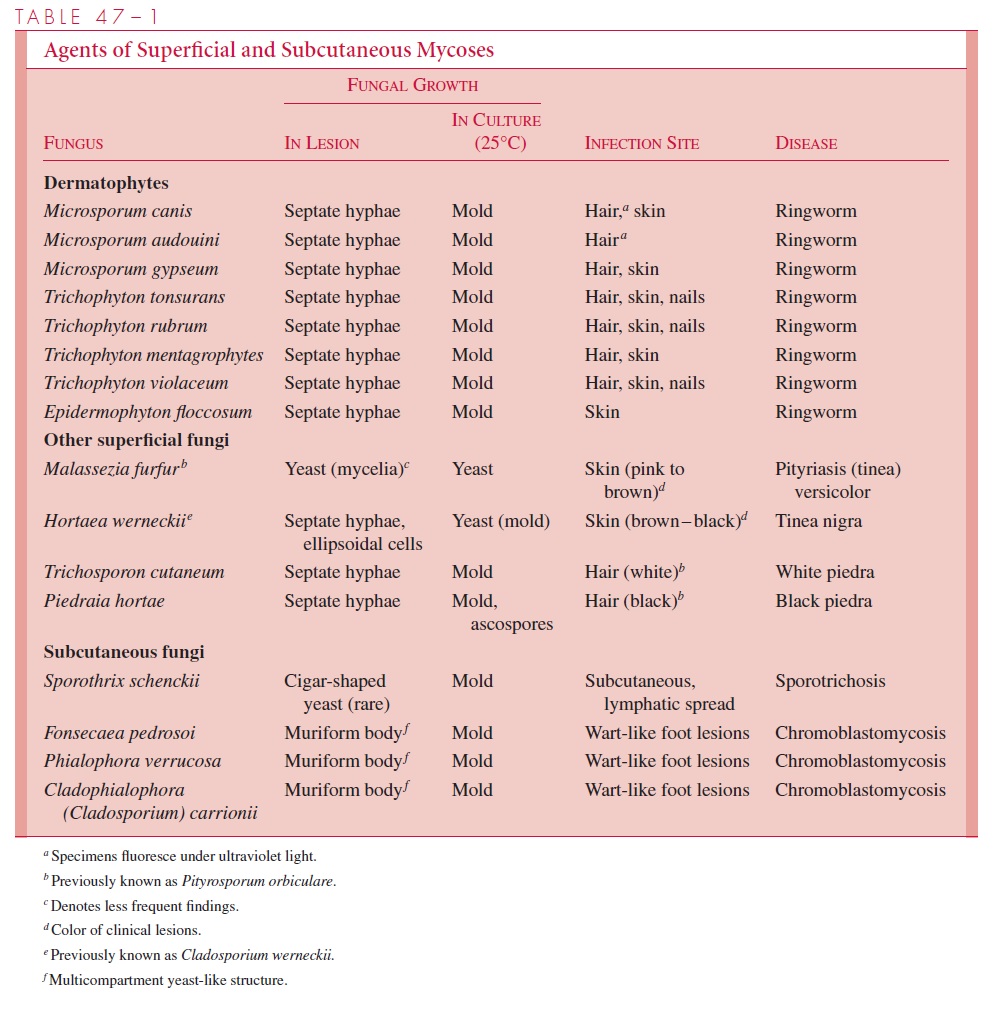
Dermatophyte infections range from inapparent colonization to chronic progressive erup-tions that last months or years, causing considerable discomfort and disfiguration. Derma-tologists often give each infection its own “disease” name, for example, tinea capitis (scalp), tinea pedis (feet, athlete’s foot), tinea manuum (hands), tinea cruris (groin), tinea barbae (beard, hair), and tinea unguium (nail beds). Skin infections not included in this anatomic list are called tinea corporis (body). There are some general clinical, etiologic, and epidemiologic differences between these syndromes, but there is also considerable overlap. The primary differences between etiologic agents that infect different sites are shown in Table 47–1.
Infection of hair begins with an erythematous papule around the hair shaft, which pro-gresses to scaling of the scalp, discoloration, and eventually fracture of the shaft. Spread to adjacent hair follicles progresses in a ring-like fashion, leaving behind broken, discol-ored hairs and sometimes black dots where the hair is absent but the infection has gone into the follicle. The degree of inflammatory response markedly affects the clinical ap-pearance and, in some cases, can cause constitutional symptoms. In most cases, symp-toms beyond itching are minimal.
Skin lesions begin in a similar pattern and enlarge to form sharply delineated erythema-tous borders with skin of nearly normal appearance in the center. Multiple lesions can fuse to form unusual geometric patterns on the skin. Lesions may appear in any location, but are particularly common in moist, sweaty skin folds. Obesity and the wearing of tight apparel increase susceptibility to infection in the groin and beneath the breasts. Another form of in-fection, which involves scaling and splitting of the skin between the toes, is commonly known as athlete’s foot. Moisture and maceration of the skin provide the mode of entry.
Nail bed infections first cause discoloration of the subungual tissue, then hyperkerato-sis and apparent discoloration of the nail plate by the underlying infection follow. Direct infection of the nail plate is uncommon. Progression of hyperkeratosis and associated in-flammation cause disfigurement of the nail but few symptoms until the nail plate is so dis-lodged or distorted that it exposes or compresses adjacent soft tissue.
DIAGNOSIS
The goal of diagnostic procedures is to distinguish dermatophytoses from other causes of skin inflammation. Infections caused by bacteria, other fungi, and noninfectious disorders (psoriasis, contact dermatitis) may have similar features. The most important step is mi-croscopic examination of material taken from lesions to detect the fungus. Potassium hydroxide (KOH) or calcifluor white preparations of scales scraped from the advancing edge of a dermatophyte lesion demonstrate septate hyphae (Fig 47–1B). Examination of infected hairs reveals hyphae and arthroconidia penetrating the hair shaft. Broken hairs give the best yield. Some species of dermatophyte fluoresce, and selection of hairs for ex-amination can be aided by the use of an ultraviolet lamp (Wood’s lamp).
The same material used for direct examination can be cultured for isolation of the of-fending dermatophyte. Mild infections with typical clinical findings and positive KOH preparations are often not cultured, because clinical management is not influenced signifi-cantly by the identity of the etiologic species. Clinically typical infections with negative KOH preparations require culture. The major reason for false-negative KOH results, how-ever, is failure to collect the scrapings or hairs properly.
TREATMENT AND PREVENTION
Many local skin infections resolve spontaneously without chemotherapy. Those that do not may be treated with topical tolnaftate, allylamines, or azoles. Nail bed and more extensive skin infections require systemic therapy with griseofulvin or itraconazole and terbinafine, often combined with topical therapy. Therapy must be continued over weeks to months, and relapses may occur. Keratolytic agents may be useful for reducing the size of hyper-keratotic lesions. Dermatophyte infections can usually be prevented simply by observing general hygienic measures. No specific preventive measures such as vaccines exist.
Related Topics