Chapter: Obstetrics and Gynecology: Sexual Assault and Domestic Violence
Sexual Assault
SEXUAL ASSAULT
Sexual
assault is defined legally as involving any genital, oral, or anal penetration
by a part of the accused’s body or by an object, using force or without
consent. Criminal sexual assault, orrape, often is further
characterized to include acquaintance rape, date rape, “statutory rape,” child
sexual abuse, and in-cest. These terms generally relate to the age of the
victim and her relationship to the abuser.
Each year, some 365,000 women in
the United States experience sexual assault, rape, or attempted rape. An
es-timated 1 in 6 women have experienced sexual assault in their lifetimes.
However, most do not file a complaint or report and, thus, its true prevalence
is unknown. In the years between 1992 and 2000, 63% percent of completed rapes,
65% of attempted rapes, and 74% of completed and attempted sexual assaults
against females were not re-ported to the police. Because of the complex
problems caused by sexual assault, treatment is best managed by a
multidisciplinary team that fulfills the following roles:
·
Care for
the victim’s emotional needs, acute and (ifpossible within the
constraints of the healthcare system) long-term
·
Evaluation
and treatment of medical needs, acuteand follow-up
·
Collection
of forensic specimens and preparation of arecord
acceptable for healthcare and in the legal process
Definitions and Types of Sexual Assault
Sexual assault occurs in all age,
racial, and socioeconomic groups; the very young, handicapped, and the very old
are particularly susceptible. Although the act may be com-mitted by a stranger,
in many cases it is committed by an acquaintance.
Some situations have been defined
as variants of sexual assault. Marital
rape is defined as forced coitus or related sexual acts within a marital
relationship without the consent of a partner; it often occurs in conjunction
with and as part of physical abuse in cases of domestic or intimate-partner
violence.
Date rape
or
acquaintance rape is another manifes-tation of intimate-partner violence.
In this situation, a woman may voluntarily participate in sexual play, but
coitus occurs, often forcibly, without her consent. Date rape often goes
unreported, because the woman may think that she contributed to the act by
participating up to a point or that she will not be believed. Lack of consent
also may occur in situations where cognitive function is im-paired by
flunitrazepam, alcohol, or other drugs; sleep; in-jury with unconsciousness; or
developmental delay.
All states have statutory rape
statutes criminalizing sexual intercourse with a girl younger than a specific
age, because she is defined, by statute, as being incapable of consenting. Many
states also have laws addressing aggra-vated
criminal sexual assault, which has the following attributes: weapons are
used, lives are endangered, or phys-ical violence is inflicted; the act is
committed in relation-ship to another felony; or the woman is older than 60
years, physically handicapped, or mentally retarded.
Management
The medical and health consequences of sexual assault are both short- and long-term. Clinicians should be aware that their practices will include women with a history of sexual assault, and they should be familiar with both the short- and long-term sequelae. All patients should be screened for a history of sexual assault. Most women with a history of sexual assault will not have reported it to a nonpsychiatric physician. Yet, women with a history of assault are more likely to present with chronic pelvic pain, dysmenorrhea, menstrual cycle disturbances, and sexual dysfunction than are women without such a history.
Clinicians evaluating women in
the acute phase who have experienced sexual assault have a number of
responsi-bilities, both medical and legal (Table 48.1). They should be familiar
with state rape and assault laws, and comply with any legal requirements
regarding reporting and the collec-tion of evidence. They also must be aware
that every state and the District of Columbia require physicians to report
child abuse, including sexual assault against children and adolescents.
Physicians should be familiar with any state laws regarding the reporting of
statutory rape. Additionally, physicians should be aware of local protocols
regarding the use of specially trained sexual assault forensic examiners or
sexual assault nurse examiners. Specific responsibilities are determined by the
patient’s needs and by state law.
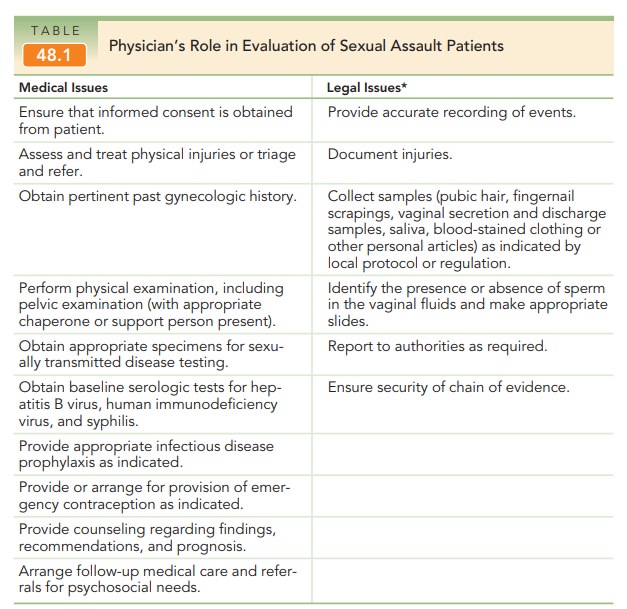
The clinician should provide
medical and counseling services, inform the patient of her rights, refer her to
legal assistance, and help her develop prevention strategies to avoid future
assault. Many jurisdictions and several clinics have developed a sexual assault
assessment kit, which lists the steps necessary and the items to be obtained so
that as much information as possible can be prepared for forensic purposes.
Many clinics have nurses who are trained to col-lect needed samples and
information. If these individuals are available, it is appropriate to request
their assistance. Rape crisis counselors and centers also can provide valuable
support. In addition, the clinician must assess and treat all injuries, perform
sexually transmitted disease (STD) screen-ing, and provide prophylaxis against
infectious diseases and unintended pregnancy.
INITIAL CARE
When a
woman who has experienced sexual assault communicates with the physician’s
office, emergency room, or clinic before pre-senting for evaluation, she should
be encouraged to come immedi-ately to a medical facility and be advised not to
bathe, douche, urinate, defecate, wash out her mouth, clean her fingernails,
smoke, eat, or drink.
In recent years, there has been a
trend toward the im-plementation of hospital-based programs to provide acute
medical and evidentiary examinations by sexual assault nurse examiners or
sexual assault forensic examiners. Physi-cians play a role in the policy and
procedure development and implementation of these programs, and serve as
sources for referral, consultation, and follow-up. In some parts of the
country, however, obstetrician–gynecologists will still be the first point of
contact for evaluation and care in the acute aftermath of a sexual assault. In
addition, virtually all obstetrician–gynecologists will be called on to perform
evaluations and, if conducting screening for history of sex-ual assault, will
realize the utility of this information to the conduct of primary-care and
specialty-care practice.
In an optimal situation, the
woman is able to seek care in a facility where there is a trained
multidisciplinary team. A team member should remain with the patient to help
provide a sense of safety and security and, thereby, begin the therapeutic
process, including, specifically, assurance of the patient’s lack of guilt. The patient should be encouraged,in a
supportive, nonjudgmental manner, to talk about the assault and her feelings. Treatment
for life-threatening traumaneeds to begin immediately. Such trauma is uncommon,
although minor trauma is seen in one-fourth of victims. Even in life-threatening
situations, any sense of control that can be given the patient is helpful.
Obtaining consent for treatment is not only a legal requirement, but also an
important aspect of the emotional care of the patient, by helping her
participate in regaining control of her body and her circumstances.
Although patients are commonly
reluctant to do so, they should be gently encouraged to work with the police,
because such cooperation is clearly associated with im-proved emotional
outcomes for victims.
History taking about a sexual
assault is necessary to gain medical and forensic information, and is as well
an important therapeutic activity. Recalling the details of the assault in the
supportive environment of the healthcare setting allows the victim to begin to
gain an understand-ing of what has happened and to start emotional healing (see
Box 48.1.).
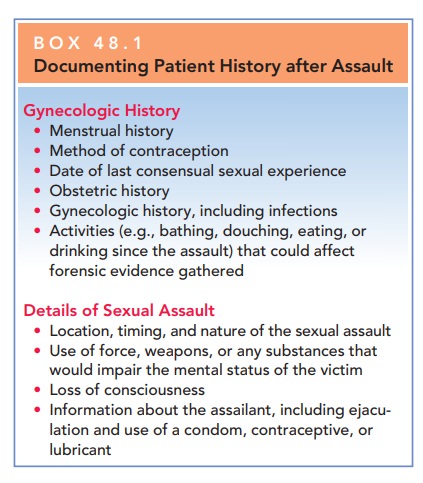
Box 48.1
Documenting Patient History after Assault
Gynecologic History
Menstrual history
Method of contraception
Date of last consensual sexual experience
Obstetric history
Gynecologic history, including infections
Activities (e.g., bathing, douching, eating, or drinking since the assault) that could affect forensic evidence gathered
Details of Sexual Assault
Location, timing, and nature of the sexual assault
Use of force, weapons, or any substances that would impair the mental status of the victim
Loss of consciousness
Information about the assailant, including ejacu-lation and use of a condom, contraceptive, or lubricant
Victims of sexual assault should
be given a complete general physical examination, including a pelvic
examina-tion. Forensic specimens should be collected, and cultures for STDs
should be obtained. When collecting forensic specimens, it is critical that the
clinician follow the direc-tions on the forensic specimens kit. These specimens
are kept in a health professional’s possession or control until turned over to
an appropriate legal representative. This “protective custody” of the specimens
ensures that the correct specimen reaches the forensic laboratory and is called
the “chain of evidence.”
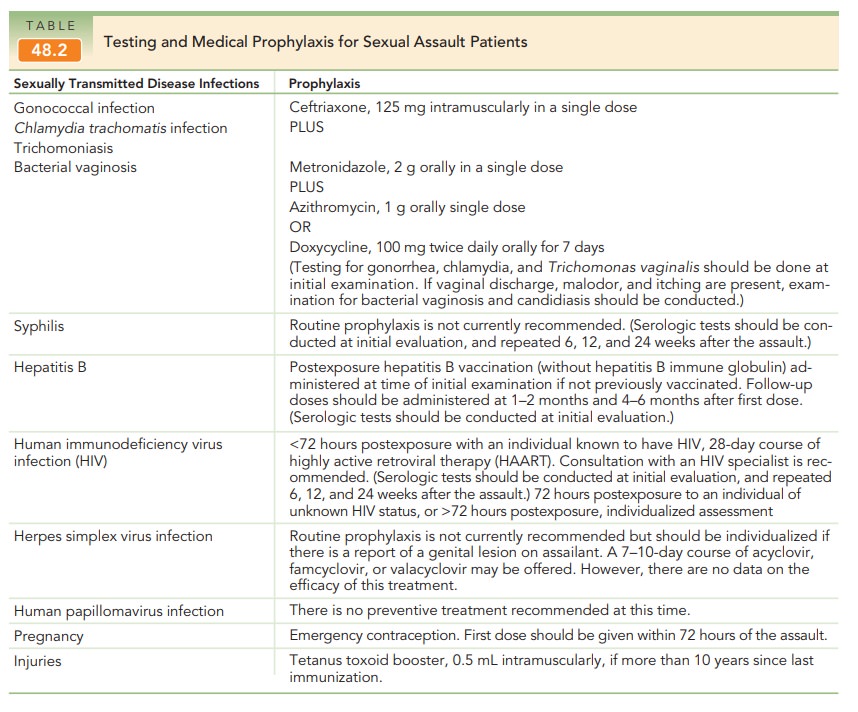
Initial laboratory tests should
include cultures from the vagina, anus, and pharynx for STDs. Collection of
serum for rapid plasma reagin (RPR) for syphilis, hepati-tis antigens, and
human immunodeficiency virus (HIV) are needed. Urinalysis, culture and
sensitivity, as well as a pregnancy test for menstrual-age women (regardless of
contraceptive status) are collected. Antibiotic
prophy-laxis should be offered to all adult patients. Emergency contraception should be offered and is described on
contraception (see Table 48.2).
Within 24
to 48 hours of disclosure and initial treatment, victims should be contacted by
phone or seen for an immediate post-treatment
evaluation. At this time, emotional or physi-cal problems are
managed and follow-up appointments arranged. Potentially serious problems, such
as suicidal ideation, rectal bleeding, or evidence of pelvic infection, may go
unrecognized by the victim during this time because of fear or continued
cognitive dysfunction. Specific questions must be asked to ensure that such
problems have not arisen.
SUBSEQUENT CARE
At the 1-week follow-up visit, a
general review of the pa-tient’s progress is made and any specific new problems
ad
The next routine visit
is at 6 weeks, when a com-plete evaluation, including physical examination,
repeat cultures for sexually transmitted diseases, and a repeat RPR is
performed. Another visit at 12 to 18 weeks may be indicated for repeat HIV
titers, although the current un-derstanding of HIV infection does not allow an
estimate of the risk of exposure for sexual assault victims. Each vic-tim
should receive as much counseling and support as is necessary, with referral to
a long-term counseling pro-gram if needed.
If the physician is not directly
involved in the acute care of the victim, it is helpful for him or her to
obtain records of the patient’s emergency evaluation. These enable the
physician to be certain that all appropriate testing was per-formed and to
provide the patient with full results. Patients may be disturbed to learn that
the results of their forensic evaluation are usually not provided to their
physician. In this situation, it is helpful to refer the patient to local legal
or police authorities, who can also be helpful in answering patients’ questions
about the health status of the assailant and whether the assailant was
apprehended.
Emotional Issues
A woman who is sexually assaulted
loses control over her life during the period of the assault. Her integrity,
and sometimes her life, is threatened. She may experience in-tense anxiety,
anger, or fear. After the assault, a “rape-trauma” syndrome commonly occurs,
comprising two phases:
ACUTE PHASE (IMMEDIATE RESPONSE)
·
May last for hours or days
·
Characterized by distortion or
paralysis of the individ-ual’s coping mechanisms
·
Outward responses vary from
complete loss of emo-tional control to an apparently well-controlled behavior
pattern.
·
Signs may include generalized
pain throughout the body; headache; eating and sleep disturbances; and
emotional symptoms, such as depression, anxiety, and mood swings.
DELAYED (OR ORGANIZATION) PHASE
·
Characterized by flashbacks,
nightmares, and phobias as well as somatic and gynecologic symptoms
·
Often occurs months or years
after the event, and may involve major life adjustments
This rape-trauma syndrome is
similar to a grief reaction in many respects. As such, it can only be resolved
when the victim has emotionally worked through the trauma and personal loss
related to the event and replaced it with other life experiences. An inability to think clearly or
rememberthings such as her past medical history, termed “cognitive dys-function,” is a particularly distressing aspect of
the syndrome.The involuntary loss of cognition may raise fears of “being
crazy” or of being perceived as “crazy” by others. It is also frustrating for
the healthcare team, unless it is recognized that this is an involuntary,
temporary, and understandable reaction to the emotionally intolerable nature of
the sexual assault and not a willful action.
Those who have experienced
physical and sexual as-sault also are at great risk of developing posttraumatic
stress disorder. Clusters of symptoms may not appear for months or even years
after a traumatic experience. These clusters are typical symptom categories
associated with posttraumatic stress disorder, including:
·
Reliving the event
·
Experiencing flashbacks,
recurring nightmares, and, more specifically, intrusive images that appear at
any time
· Extreme
emotional or physical reactions, including shak-ing, chills, palpitations, or
panic reactions, often accom-pany vivid recollections of the attack.
Avoiding
reminders of the event constitutes another symp-tom cluster in posttraumatic
stress disorder. These women become emotionally numb, withdrawing from friends
and family and losing interest in everyday activities. There may be an even
deeper reaction of denial of awareness that the event actually happened.
Symptoms such as easy startling, being hypervigilant, irritability, sleep disturbances, and lack of concentration are part of a third symptom cluster known as hyper-arousal. These women often will have a number of co-occurring conditions, such as depression, dissociative disorders (los-ing conscious awareness of the present, or “zoning out”), addictive disorders, and many physical symptoms.
Related Topics