Chapter: Obstetrics and Gynecology: Sexual Assault and Domestic Violence
Domestic Sexual Violence
DOMESTIC VIOLENCE
Domestic violence is reported by
over 25% of women at some time during their lives and is a significant source
of illness and injury to women.
Definition
Domestic
violence refers to violence perpetrated withinthe context of
family or intimate relationships. Family members include parents, siblings, and
other blood rela-tives, as well as legal relatives such as stepparents,
in-laws, and guardians. Violence that occurs between current or for-mer
partners is referred to as intimate-partner
violence and includes male abuse by female partners and violence be-tween
partners in lesbian, gay, bisexual, and transgendered relationships.
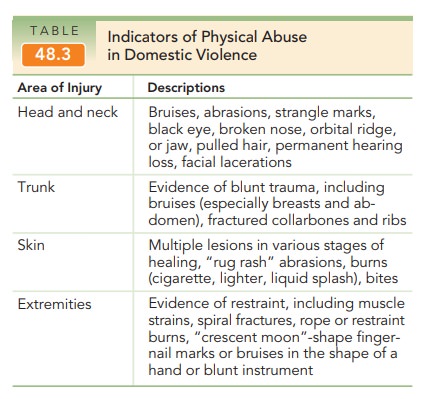
Domestic violence may involve one or more of three pre-sentations. Physical abusesuch as hitting, slapping, kick-ing, and choking, is the most obvious presentation. It is suspected with evidence of trauma, especially to the head and neck or trunk associated with a history of violence, or when an explanation of the trauma doesn’t seem appro-priate (Table 48.3). Unfortunately, pregnancy appears to be a period of greater risk for such episodes. Sexual abuse is another presentation of domestic violence. The third pre-sentation is emotional, financial, or psychological abuse,neglect, or threat, and is often traumatic and/or long-standing. Examples include undermining of self-worth, deprivation of sleep or emotional support, repetitive un-predictability of response to life situations, threats, de-struction of personal property or the killing of pets, lies, manipulation of friends, and interference in the work-place. Domestic violence is usually cyclic and repetitive, with periods of calm alternating with periods of rapidly increasing tensions or violence, the latter often increasing in severity with each iteration of the cycle.
Screening: Risk Factors
Recognition
is the first, most important, and most often a missed issue. When
domestic violence is suspected, compassionateand thoughtful discussion with the
possible victim, as well as attention to any physical injury, is requisite. All
patients should be asked about violence in their lives as part of the routine
health history. Although all women are at risk for abuse, certain life
experiences and circumstances may place some women at greater risk (Box 48.3).
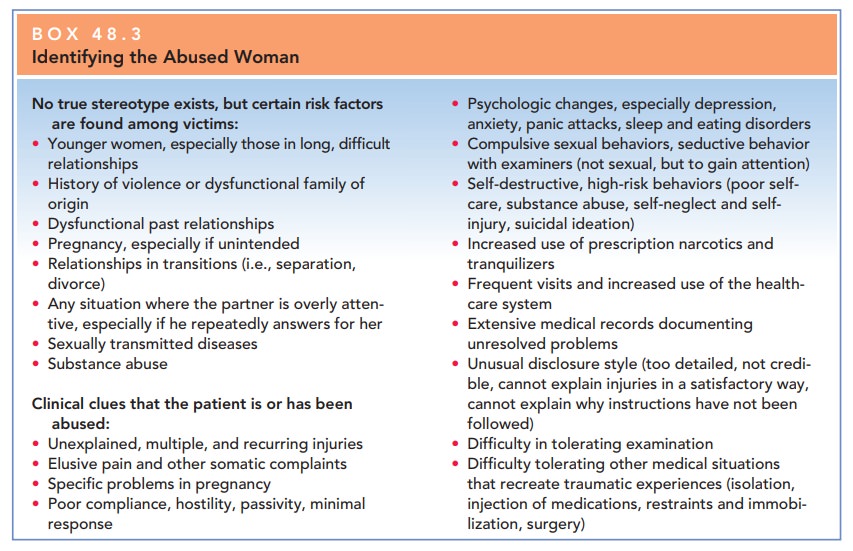
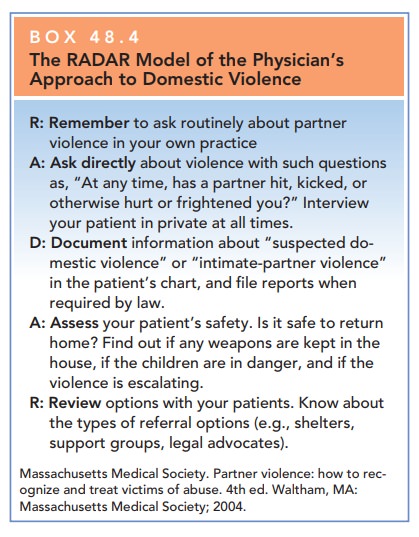
The clinician’s role is 1) to
know the signs and symp-toms of intimate-partner violence, 2) to ask all
patients about past or present exposure to violence, 3) to intervene and refer
as appropriate, and 4) to assess the patient’s risk of danger (Box 48.4).
Counseling
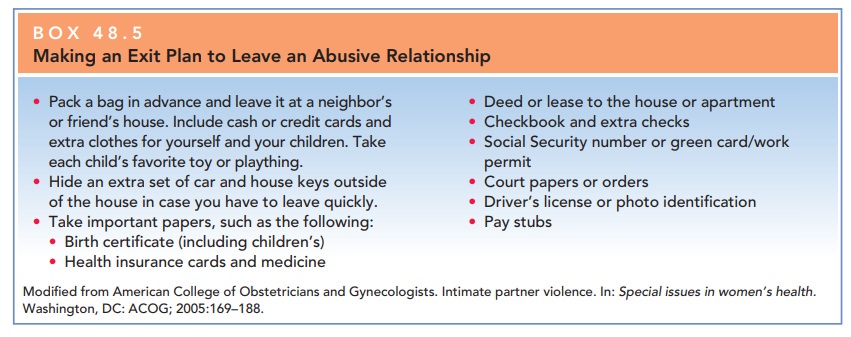
If the patient will be returning
to an unsafe home, safety planning should be conducted, and referrals to
service agencies in the community should be provided. Women can be encouraged
to call a woman’s shelter for more help
Box 48.4
The RADAR Model of the Physician’s Approach to Domestic Violence
Remember to ask routinely about partner
violence
in your own practice
Ask directly about violence with such questions as, “At any time, has a
partner hit, kicked, or otherwise hurt or frightened you?” Interview your
patient in private at all times.
Document information about “suspected do-mestic violence” or
“intimate-partner violence” in the patient’s chart, and file reports when
required by law.
Assess your patient’s safety. Is it safe to return home? Find out if any
weapons are kept in the house, if the children are in danger, and if the violence
is escalating.
Review options with your patients. Know about the types of referral options (e.g., shelters, support groups, legal advocates).
Related Topics