Chapter: Obstetrics and Gynecology: Sexual Assault and Domestic Violence
Child Sexual Assault
CHILD SEXUAL ASSAULT
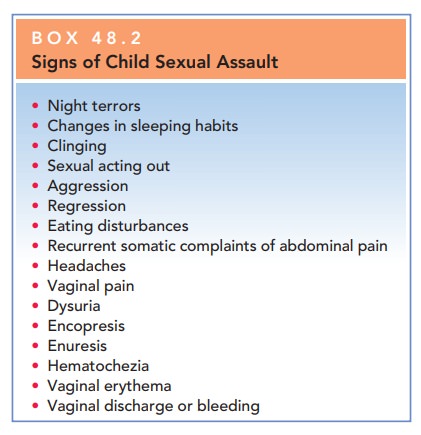
Ninety percent (90%) of child victimization is by par-ents, family members, or family friends; “stranger rape” is relatively uncommon in children. It is extremely impor-tant to know who the perpetrator is and how the child sus-tained the injury, so that the child can be removed from an unsafe environment. Box 48.2 shows behavioral and physical signs and symptoms commonly associated with child sexual abuse.
Assessment/Examination
Because the assessment of a child for sexual abuse involves specific skills and has the potential for legal challenge, the individual who undertakes this evaluation should have sig-nificant experience in this area.
This assessment
usually is done by pediatricians and is beyond the skills of most general
gynecologists. Awareness of and sensitivity to the issues, special needs, and
circumstances of the child are important for obstetrician–gynecologists who are
consulted to treat an injury to the pelvic floor. In many cities, a child abuse
team consisting of trained experts and including physicians, social workers,
and counselors is available to perform the assessment.
The sexual abuse evaluation
begins with an interview of the caretaker and the child. Unless the child
refuses to leave the caretaker, the child should be interviewed pri-vately to
obtain specific details of the abuse. Questioning should be nondirect to elicit
spontaneous responses such as time and location of the abuse, description of
the scene, name and description of the perpetrator, and type of sex-ual acts.
The child’s statements should be recorded verba-tim; electronic interviews are
helpful so that the child does not have to describe the abuse repeatedly. Good
docu-mentation of the interview is critical in the prosecution of sexual abuse
cases because, in many instances, the patient’s statement is the only evidence
that the abuse occurred. Documentation of the specific names the child uses for
her genitalia is recommended to help others understand the context of her
statements.
The urgency of an evaluation of sexual abuse depends on how soon after the event the child is brought in for care. If the child presents within 72 hours of the last episode of abuse, the physician should immediately arrange for eval-uation of the child and focus on collection of forensic evi-dence. However, fewer than 10% of child sexual abuse cases are reported within 72 hours. In cases that are re-ported after 72 hours, the patient should be referred to the nearest sexual abuse center, where more resources are available to conduct the evaluation.
MANAGEMENT
In the treatment of a child who
is the victim of sexual abuse, management should focus (as applicable) on
repair of injuries, treatment of STDs, prevention of pregnancy, protection
against further abuse, and psychologic support for the patient and her family.
Superficial injuries (e.g., bruises, edema, local irritation) resolve within a
few days and require only meticulous perineal hygiene. In some patients with
extensive skin abrasions, broad-spectrum antibiotics should be given as
prophylaxis. Small vulvar hematomas usually can be controlled by pressure with
an ice pack, and even massive swelling of the vulva usually subsides promptly
when cold packs and external pressure are applied. Injuries to the vagina or
rectum may present surgical difficulties because of the small size of the
organs involved. More extensive penetrative vaginal and anal injuries require
thorough radiographic and anesthetic examination to rule out intraabdominal
penetration.
Related Topics