Chapter: Essentials of Psychiatry: Substance Abuse: Sedative, Hypnotic, or Anxiolytic Use Disorders
Risk Factors for Low-dose Benzodiazepine Withdrawal
Risk Factors for Low-dose
Benzodiazepine Withdrawal
Some drugs or medications may facilitate
neuroadaptation by increasing the affinity of benzodiazepines for their
receptors. Phenobarbital, for example, increases the affinity of diazepam to
benzodiazepine receptors and prior treatment with phenobarbital has been found
to increase the intensity of chlordiazepoxide (45 mg/day) withdrawal symptoms.
Patients at increased risk for development of the low-dose withdrawal syndrome
are those with a family or personal history of alcoholism, those who use
alcohol daily and those who concomitantly use other sedatives. Case–control
studies suggest that patients with a history of ad-diction, particularly to
other sedative–hypnotics, are at high risk for low-dose benzodiazepine
dependence. The short-acting, high-milligram-potency benzodiazepines appear to
produce a more intense low-dose withdrawal syndrome.
Treatment of Protracted Benzodiazepine Withdraw
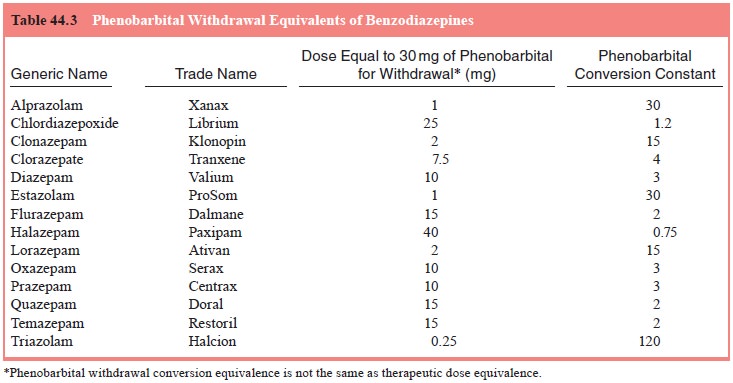
Phenobarbital conversions based on Table 44.3 are
not adequate to suppress symptoms. For example, someone discontinuing 20 mg of
diazepam would have a computed phenobarbital con-version of 60 mg. In managing
low-dose withdrawal, an ap-proach is to begin with about 200 mg/day of
phenobarbital and then taper the phenobarbital slowly as tolerated. If
palpitations or other symptoms of autonomic hyperactivity are bothersome,
beta-adrenergic blockers, such as propranolol or 2-adrenergic agonists, such as
clonidine, may be useful adjuncts. Reports on the use of clonidine to reduce
benzodiazepine withdrawal sever-ity have yielded mixed results.
Related Topics