Chapter: Essentials of Psychiatry: Substance Abuse: Sedative, Hypnotic, or Anxiolytic Use Disorders
Additional Treatment Considerations - Disorders of Sedative–Hypnotics
Additional Treatment
Considerations
Psychiatric Comorbidity
Most patients who are being prescribed long-term benzodiazepine therapy have underlying major depressive disorder, panic disorder or GAD. The clinical dilemma is deciding which patients are receiving appropriate maintenance therapy for a chronic psy-chiatric condition. Physical dependence on benzodiazepines may be acceptable if the patient’s disabling anxiety symptoms are ameliorated. The reason for the patient’s request for benzo-diazepine withdrawal from long-term, stable dosing should be carefully explored. Valid reasons to discontinue benzodiazepine treatment include: 1) breakthrough of symptoms that were previously well controlled; 2) impairment of memory or other neurocognitive functions; and 3) abuse of alcohol, cocaine, or other medications.
Patients with severe underlying psychiatric
disorders may have unrealistic hopes of becoming medication-free. Often the
origin of request for benzodiazepine withdrawal comes from concerned friends or
relatives.
Abuse Potential of Benzodiazepines
Most people do not like the subjective effects of
benzodiazepines, especially in high doses. Even among drug addicts, the
benzodi-azepines alone are not common intoxicants. They are, however, widely
used by drug addicts to self-medicate opiate withdrawal and to alleviate the
side effects of cocaine and amphetamines. Patients receiving methadone
maintenance use benzodiazepines to boost (enhance) the effects of methadone.
Some alcoholic patients use benzodiazepines either in combination with alcohol
or as a second-choice intoxicant, if alcohol is unavailable. Fat-soluble
benzodiazepines that enter the CNS quickly are usually the benzodiazepines
preferred by addicts.
Addicts whose urine is being monitored for
benzodi-azepines prefer benzodiazepines with high milligram potency, such as
alprazolam or clonazepam. These benzodiazepines are excreted in urine in such
small amounts that they are of-ten not detected in drug screens, particularly
with thin-layer chromatography.
Treatment of High-dose Benzodiazepine Dependence
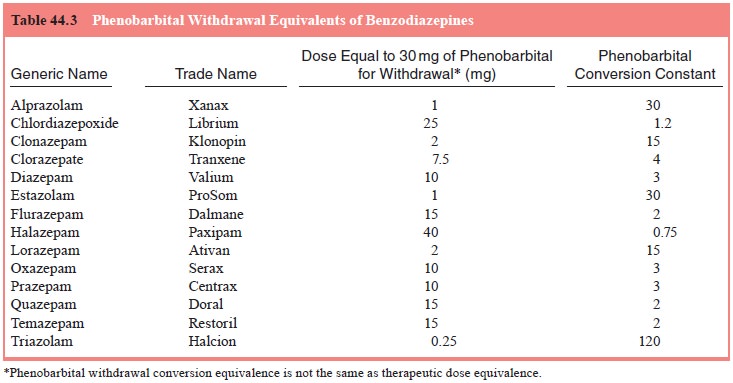
For high-dose benzodiazepine dependence, the
pharmacologi-cal treatment strategy is the same as that for barbiturates. The
phenobarbital conversion equivalents are shown in Table 44.3. The dose
conversions computed using Table 44.3 prevent the emergence of severe
withdrawal of the classic sedative–hypnotic types. Some patients who take high
doses of benzodiazepines, or even therapeutic doses for months to years, may
have prolonged withdrawal symptoms.
Low-dose Benzodiazepine Withdrawal Syndromes
Many people who have taken benzodiazepines in
therapeutic doses for months to years can abruptly discontinue the drug
with-out developing withdrawal symptoms. But other patients, taking similar
amounts of a benzodiazepine develop symptoms ranging from mild to severe when
the benzodiapine is stopped or when the dosage is substantially reduced.
Characteristically, patients toler-ate a gradual tapering of the benzodiazepine
until they are at 10 to 20% of their peak dose. Further reductions in
benzodiazepine dose then cause patients to become increasingly symptomatic. In
addition medicine literature, the low-dose withdrawal may be called
therapeutic-dose withdrawal, normal-dose withdrawal, or benzodiazepine
discontinuation syndrome. The symptoms can ultimately be categorized as symptom
reemergence, symptom rebound, or a prolonged withdrawal syndrome.
Many patients experience a transient increase in
symptoms for 1 to 2 weeks after benzodiazepine withdrawal. The symptoms are an
intensified return of the symptoms for which the benzodiazepine was prescribed.
This transient form of symptoms intensification is called symptom rebound. The term comes from sleep research in which
rebound insomnia is commonly observed after sedative–hypnotic use. Symptom
rebound lasts a few days to weeks after discontinuation Symptom rebound is the
most common withdrawal consequence of prolonged benzodiazepine use.
The symptoms for which the benzodiazepine has been
taken may return to the same level as before benzodiazepine therapy. This is
called symptom reemergence (or recrudescence). In other words, the patient’s
symptoms, such as anxiety, insom-nia, or muscle tension, that had abated during
benzodiazepine treatment return.
The reason for making a distinction between symptom
re-bound and symptom reemergence is that symptom reemergence suggests that the
original symptoms are still present and must be treated. Symptom rebound is a
transient withdrawal syndrome that will disappear over time.
A few patients experience a severe, protracted withdrawal
syndrome that includes symptoms (e.g., paresthesia and psycho-sis) that were
not present before. This withdrawal syndrome has generated much of the concern
about the long-term safety of the benzodiazepine
Related Topics