Chapter: Essentials of Psychiatry: Substance Abuse: Sedative, Hypnotic, or Anxiolytic Use Disorders
Acute Intoxication with Sedative–Hypnotics
Acute Intoxication with
Sedative–Hypnotics
The acute toxicity of sedative–hypnotics consists
of slurred speech, incoordination, ataxia, sustained nystagmus, impaired
judgment and mood lability. When taken in large amounts sedative–hypnotics
produce progressive respiratory depression and coma. The amount of respiratory
depression produced by the benzodiazepines is much less than that produced by
the barbiturates and other sedative–hypnotics. Consistent with its general
approach, the DSM-IV-TR diagnosis of intoxication requires “clinically
significant maladaptive behavioral or psychological changes” developing after
drug use in addition to the signs and symptoms of acute toxicity.
Dependence
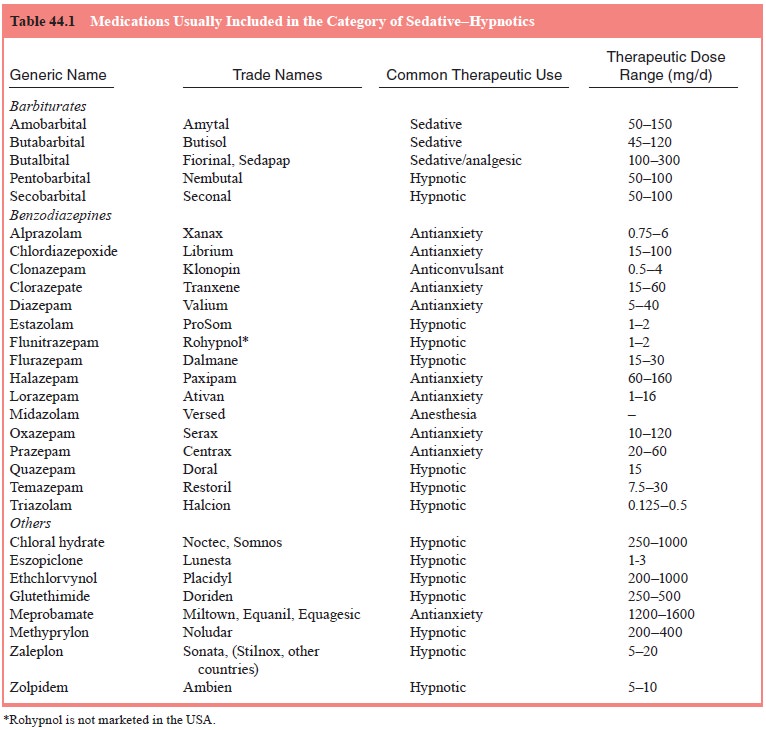
Sedative–hypnotics can produce tolerance and
physiological dependence. Physiological dependence can be induced within
several days with continuous infusion of anesthetic doses. Pa-tients who are
taking barbiturates daily, for example, for a month or more above the upper
therapeutic range listed in Table 44.1 should be presumed to be physically
dependent and in need of medically managed detoxification.
Withdrawal Syndrome
The withdrawal syndrome arising from the
discontinuation of short-acting sedative–hypnotics is similar to that from
stopping or cutting down on the use of alcohol. Signs and symptoms of
sedative–hypnotic withdrawal include anxiety, tremors, night-mares, insomnia,
anorexia, nausea, vomiting, postural hypo-tension, seizures, delirium and
hyperpyrexia. The syndrome is qualitatively similar for all sedative–hypnotics;
however, the time course of symptoms depends on the particular drug. With
short-acting sedative–hypnotics (e.g., pentobarbital, secobarbi-tal,
meprobamate, oxazepam, alprazolam and triazolam), with-drawal symptoms
typically begin 12 to 24 hours after the last dose and peak in intensity
between 24 and 72 hours (symptoms may develop more slowly in patients with
liver disease or in the elderly because of decreased drug metabolism). With
long-acting drugs (e.g., phenobarbital, diazepam and chlordiazepox-ide),
withdrawal symptoms peak on the fifth to eighth day. The withdrawal delirium
may include confusion, visual and auditory hallucinations. The delirium
generally follows a period of insom-nia. Some patients may have only delirium;
others only seizures; and some may have both delirium and convulsions.
Iatrogenic Dependence
Patients treated for months to years with
benzodiazepines and other sedative–hypnotics may become physically dependent on
sedative–hypnotics. The possibility of physical dependence should be discussed
with the patient and, in some cases, the pa-tient’s family. The distinction
between physical dependence as a process of neuroadaptation and physical dependence
as a com-ponent of a substance-use disorder should be explained in detail.
Patients need to be advised against abruptly stopping the medica-tion because
of the possibility of developing severe withdrawal symptoms, including
seizures.
Related Topics