Chapter: Ophthalmology: Visual Pathway
Retrochiasmal Lesions
Retrochiasmal Lesions
Etiology:
Retrochiasmal lesions may result from a wide variety ofneurologicdisorders such as tumors,
vascular insults, basal meningitis, aneurysms of theposterior communicating
artery, abscesses, injuries (such as a contrecoup injury to the occipital
lobe), and vasospasms (in an ocular migraine).
Symptoms, diagnostic considerations, and clinical picture:
Visual fieldtesting in particular will provide
information on the location of the lesion. Perimetry
is therefore a crucial diagnostic study.Bilateral
simultaneous visualfield defects are common to all retrochiasmal lesions of
the visual pathway.Often these defects will be incongruent.
Homonymous visual field defects are the result of a retrochiasmal lesion.
Lesions of the optic tract and the lateral geniculate body.Because the nervefibers are concentrated in a
very small space, the visual field defect that occurs typically in these
lesions is homonymous hemianopsia. Lesions on the right side produce visual
field defects in the left half of the visual field and vice versa. Partial
primary atrophy of the optic nerve may occur as the third neuron is affected,
which extends from the retina to the lateral geniculate body. An afferent pupillary defect on the side
opposite the lesion will be present. The cause of this defect is not known.
Special forms.
Cortical blindness.Bilateral lesions of the visual cortex, especially injuries,can
produce both temporal and nasal visual field defects with normal pupil-lary light reaction and normal optic disk findings.
Visual agnosia.Where the association areas of the brain are damaged, asoften
occurs in lesions of the parietal lobe or marginal visual cortex, the patient
can see but is unable to interpret or classify visual information. Examples of
this include alexia (acquired inability to comprehend written words) and color
agnosia (inability to distinguish colors).
Other symptoms and findings.Depending on the underlying disorder, thesemay include headache,
nausea, vomiting, and papilledema. A differential diagnosis requires CT and MRI
studies.
Lesions of the optic radiations.Thevisual field defectsassumemany differentforms due to the wide
spread of the optic radiations. Injuries to both the tem-poral and parietal
lobes typically produce homonymous
hemianopsia. Injuries primarily involving the temporal lobe produce
homonymous superior quad-rantic
anopsia; injuries primarily involving the parietal lobe produce homo-nymous inferior quadrantic anopsia. Pupillary
findings are normal because the lesion affects the fourth neuron. Approximately
30% of all cases involve an afferent
pupillary defect on the side opposite the lesion. The cause of this
defectis not known.
Lesions of the visual cortex.The visual field defects, like the lesions of thevisual pathway, are homonymous and hemianoptic. The macula may or may not be affected depending on the extent of the lesion.
Treatment:
Depending on the underlying disorder, the patient is referred
toeither a neurologist or neurosurgeon for treatment.
Prognosis:
The prognosis is generally poor, and the visual field defects
usu-ally do not subside.
Ocular Migraine
This is due to a transient vasospasm of
the posterior cerebral artery that supplies the visual cortex. Symptoms vary. Typically there will be a unilateral
homonymous and initially paracentral scintillating scotoma, a series of flashes
of bright light (fortification spectra), and perceptions of dazzling colors.
Headache, nausea, and vertigo also occur. Paresis of the ocular muscles (ophthalmoplegic migraine) may also
occur. Treatment: Patients should be referred to a neurologist.
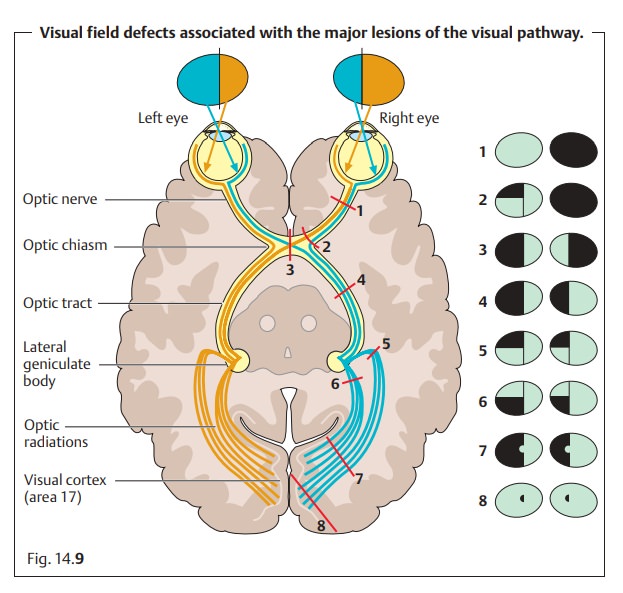
Fig. 14.9 provides a schematic overview of all major lesions of the visual pathway
with their associated visual field defects.
Related Topics