Chapter: Ophthalmology: Visual Pathway
Chiasmal Lesions
Chiasmal Lesions
Anatomy:
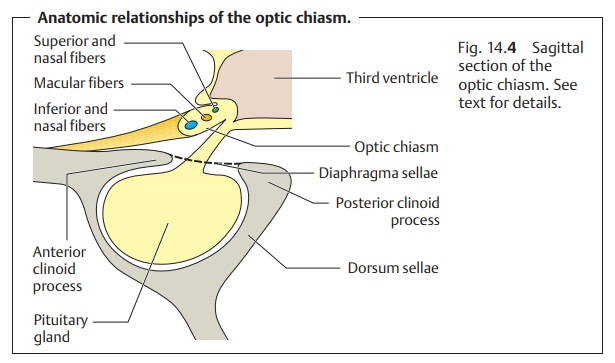
The optic chiasm and the optic nerves (Fig. 14.4) lie on the dia-phragma sellae, a
dural fold that forms the roof of the sella turcica.
The pituitary gland in the sella turcica lies inferior to the chiasm. The internal carotid artery defines the lateral border of the chiasm. The hypothalamus and anterior lobe of the cerebrum are located
superior to thechiasm. Within the chiasm,
the inferior nasal fibers cross inferiorly and ante-riorly, and are therefore
most likely to be affected by pituitary
tumors. The superior nasal fibers cross posteriorly and superiorly within
the chiasm and are therefore most likely to be affected by craniopharyngiomas. The macular fibers cross in various locations
throughout the chiasm, including posteriorly and superiorly.
Etiology and corresponding visual field defects:
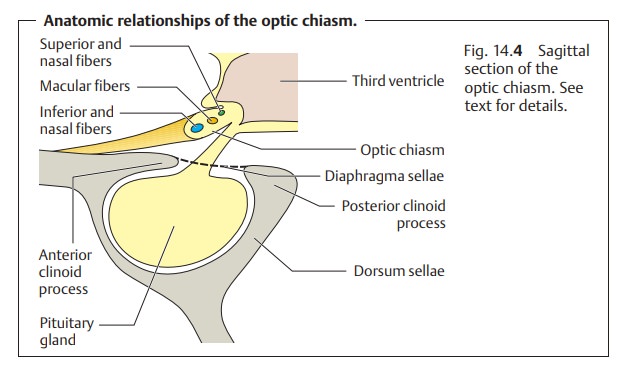
Pituitary adenomas: These are tumors that proceed from the hormone-secreting cells of the anterior lobe of the pituitary gland. As they increase in size superiorly, they reach the anterior margin of the chiasm where they com-press the inferior and nasal fibers that cross there (Fig. 14.5). This leads to an initial visual field defect in the superior temporal quadrant that may laterprogress to complete bilateral temporal hemianopsia. The visual field defect usually spreads in an asymmetrical pattern. The eye with the more severe visual field defect often exhibits the lesser central visual acuity.
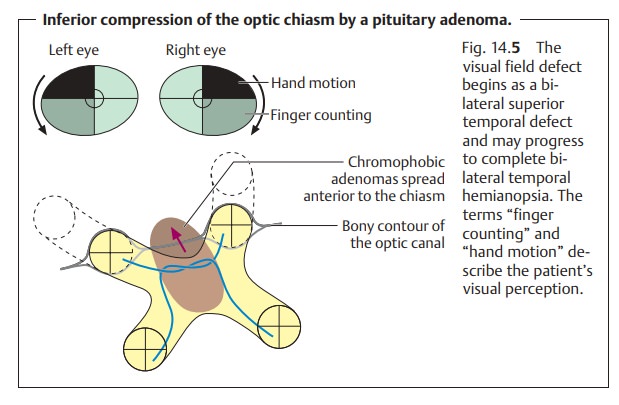
Craniopharyngiomas.These slow-growing tumors develop from tissue of thepouch of Rathke (the pituitary diverticulum) along the stem of the pituitary gland. Craniopharyngiomas compress the optic chiasm posteriorly and superiorly and therefore primarily affect the superior nasal fibers that cross there (Fig. 14.6).
The corresponding visual field defect begins in the inferior tem-poral quadrants and
then spreads into the superior temporal quadrants
Meningiomas.These are tumors that proceed from the arachnoid. They mayaffect
various different parts of the chiasm depending on the site of their origin
(Fig. 14.7). When they occur on the
tuberculum sellae, they can com-press either the optic nerve or the chiasm.
Tumors that compress the junction of the optic nerve and chiasm simultaneously
compress the fibers in the arc of Wilbrand. In addition to the ipsilateral
central scotoma, this produces a con-tralateral visual field defect in the superior temporal quadrants. Meningiomas
can also proceed from the margin of the sphenoid and compress the optic nerve.
Those that originate along the olfactory tract can lead to a loss of sense of
smell and to compression of the optic nerve.

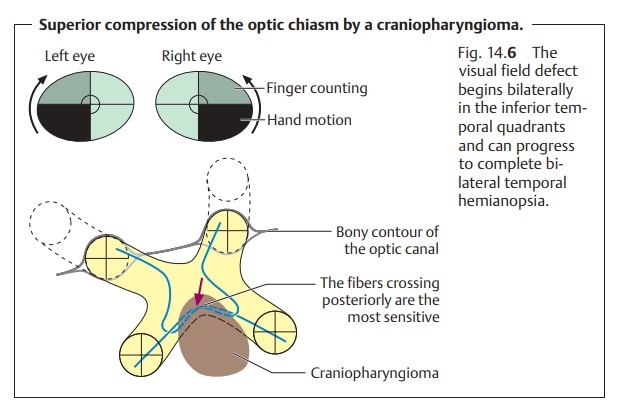
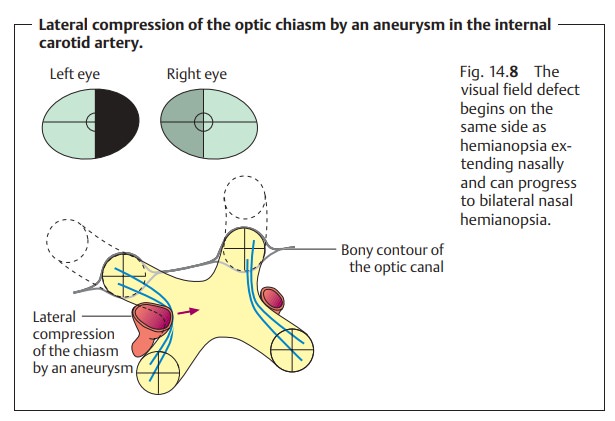
Aneurysms.Dilation of the internal carotid artery due to an aneurysm
canresult in lateral compression of optic chiasm (Fig. 14.8). The resulting visualfield
defect begins unilaterally but can become bilateral if the chiasm ispressed
against the contralateral internal carotid artery. Initially there is
ipsilateral hemianopsia extending nasally. This is followed by compression of
the contralateral side with contralateral hemianopsia that also extends
nasally.
Other changes in the chiasm.Aside from the external effects on the chiasm,changes can occur within the chiasm itself. These include gliomas, demyeli-nation, and trauma. The chiasm can also be involved in infiltrative or inflam-matory changes of the basal leptomeninges (arachnoiditis of the optic chi-asm). The resulting visual field defects are highly variable.
Symptoms, diagnostic considerations, and clinical picture:
The compres-sion of the optic nerve produces primary descending
atrophy of the opticnerve. This is associated with a more or less severe decrease in visual acuity and visual field defects (see Etiology). A
visual field defect consisting of het-eronymous bilateral temporal hemianopsia
is referred to as chiasm syn-drome.
The visual field defects in these cases are frequently incongruent.Chiasm
syndrome develops slowly and usually
represents the late stage of a pituitary adenoma or craniopharyngioma.
Heteronymous bilateral temporal hemianopsia
with decreased visual acuity and unilateral or bilateral optic nerve atrophy is
referred to as chiasm syndrome.
Bilateral temporal visual field defects are
typical for chiasmal processes. However, the many possible locations of lesions
in the region of the chiasm produce widely varying visual field defects
depending on the specific eti-ology.
Bilateral temporal visual field defects are
due to chiasmal lesions. A chiasmal lesion should always be considered in the
presence of any uncertain visual field defect.
Further diagnostic studies may be performed
after visual acuity testing, pupil-lary light reaction testing, perimetry, and
ophthalmoscopy of the fundus and optic disk. Such studies include radiographs
of the sella turcica (to detect
enlargement or destruction of the sella
turcica due to a pituitary adenoma), CT, MRI, carotid arteriography, and, in
applicable cases, endocrinologic studies.
Treatment:
This depends on the underlying cause. Neurosurgery may
beindicated or medication, such as bromocriptine for a pituitary tumor.
Prognosis:
This also depends on the underlying disorder. Ocular
functionaldeficits may subside when the disorder is promptly diagnosed and
treated.
Related Topics