Chapter: Essentials of Psychiatry: Mood Disorders: Depression
Refractory Major Depressive Disorder
Refractory Major Depressive Disorder
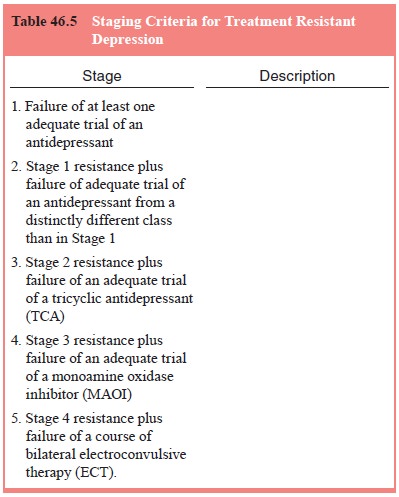
A staging system for treatment-resistant depression (TRD) has been
proposed and ranges from failure to respond to a single agent (Stage 1) to
failure of multiple treatments and electroconvulsive therapy (Stage 5; Thase
and Rush, 1995), and is presented in Ta-ble 46.5. The term refractory
depression has been proposed to de-scribe patients who have Stage 5
treatment-resistant depression.
Refractory MDD or Stage 5 in Table 46.5 is estimated to occur in up to
20% of patients. A larger percentage of patients with MDD, up to 30%, may show
only partial improvement. The concept of treatment-resistant depression or
refractory depres-sion describes this lack of response to a number of clinical
trials using optimal dosing and duration of antidepressant medication. One must
typically offer the patient a rational series of treatment trials using optimal
dosing and duration of each antidepres-sant. Many individuals consider a
patient refractory if a course of three, four, or five treatments is offered
without substantial clinical response. The standard approach to the management
of refractory depression includes increasing the antidepressant dose and
monitoring for a full 8 to 12 week course augmenting the treatment with several
augmentation strategies using an adequate combination of antidepressant drug
treatment and psychotherapy and switching to alternative somatic treatments
including ECT when indicated.
Refractory
MDD is ameliorated in the context of a caring and collaborative treatment
relationship based on a favorable ther- apeutic
alliance. Patients sometimes will undermine treatment through their own
persistent use of substances such as alcohol or lack of adherence to specific
pharmacotherapy recommenda-tions. In this context the attention to the
therapeutic alliance is particularly critical. In assessing an individual with
refractory symptoms, pharmacologic factors including pharmacokinetic
considerations, drug–drug interactions and extreme sensitivity to
antidepressant drugs must be considered.
Despite many alternative strategies, substantial morbidity and
occasional mortality are associated with refractory MDD. In addition, careful
attention to psychosocial factors associated with refractoriness is critical.
These psychosocial factors include early childhood adversity and abuse, early
family dysfunction, increased neuroticism and marked disruption in the
development of a stable sense of self.
Related Topics