Chapter: Essentials of Psychiatry: Mood Disorders: Depression
Comorbidity Depression Patterns: General Medical Conditions
Comorbidity Patterns: General Medical Conditions
Whereas a 4 to 5% current prevalence rate of MDD exists in community
samples, symptoms of depression are found in 12 to 36% of patients with a
general medical condition (Depression Guideline Panel, 1993). The rate of
depression may be higher in patients with a specific medical condition. MDD is
identified as an independent condition and calls for specific treatment when it
occurs in the presence of a general medical condition.
The Depression Guideline Panel includes four possible relationships
between depression and a general medical condi-tion: 1) depression is
biologically caused by the general medical condition; 2) an individual who
carries a genetic vulnerability to MDD manifests the onset of depression
triggered by the gen-eral medical condition; 3) depression is psychologically
caused by the general medical condition; and 4) no causal relationship exists
between the general medical condition and mood disor-der. The first two cases
warrant initial treatment directed at the general medical disorder. Treatment
is advocated for persistent depression upon stabilization of the general
medical condition. When the general medical condition causes depression,
specific treatment for the former condition is optimized, while psychi-atric
management, education and antidepressant medication are administered to treat
the depression. In cases where the two con-ditions are not etiologically
related, appropriate treatment is indi-cated for each disorder.
Stroke
Some poststroke patients manifest depression due to cerebrovas-cular
disease related to cerebral infarction in left frontal and left subcortical
brain regions. Mood disorder due to cerebrovascular disease is diagnosed when
an individual manifests a recent stroke and has significant symptoms of
depression. A point prevalence of mood disorder due to cerebrovascular disease
in poststroke patients between 10 and 27% has been documented, with an av-erage
duration of depression lasting approximately 1 year. Case reports of mood
disorder due to cerebrovascular disease in post-stroke patients suggest poor
treatment compliance, irritability and personality change (Ross and Rush,
1981).
Dementia
According to DSM-IV-TR, when symptoms of clinically signifi-cant
depressed mood accompany dementia of the Alzheimer’s Type and, in the
clinician’s judgment, the depression is due to the direct physiological effects
of the Alzheimer’s disease, mood dis-order due to Alzheimer’s disease is
diagnosed. When dementia consistent with cerebrovascular disease leads to
prominent cog-nitive deficits, focal neurological signs and symptoms,
signifi-cant impairment in functioning as well as predominant depressed mood,
vascular dementia with depressed mood is diagnosed. The distinction between
depressive disorders and dementing disor-ders is often complicated because depression
and dementia com-monly cooccur. Treatment of cooccurring depressive features
may relieve symptoms and improve overall quality of life.
Parkinson’s Disease
Fifty percent of patients with Parkinson’s disease experience a MDD
during the course of the illness. When depression occurs in this context, one
diagnoses mood disorder due to Parkinson’s disease. Active treatment of the
depressive disorder may result in improvement in the signs and symptoms of
depression with-out alleviation of the involuntary movement disorder or
cognitivechanges associated with subcortical brain disease. The underly-ing
etiology of associated dementia and depressive disorder in Parkinson’s disease
appears to involve physiologic changes in subcortical brain regions.
Diabetes
It is estimated that the prevalence of depression in treated pa-tients
with diabetes is three times as frequent as in the general population. Further,
there is no difference in the prevalence rate of depression in patients with
insulin-dependent diabetes melli-tus (Type I) in comparison to patients with
noninsulin-dependent mellitus (Type II). The symptomatic presentation of MDD in
pa-tients with diabetes is similar to patients without diabetes. Con-sequently,
full assessment of and treatment for MDD is recom-mended in patients who become
depressed during the course of diabetes. The relatively high point prevalence
rate may be due to higher detection rate in this treated population, having a
chronic illness, as well as metabolic and endocrine factors.
Coronary Artery Disease
When MDD is present, increased morbidity and mortality is reported in
postmyocardial infarction patients as well as in pa-tients having coronary
artery disease without myocardial in-farction (MI). Therefore, treatment of MDD
in patients with coronary artery disease is indicated. Prevalence estimates of
MDD in postmyocardial infarction range from 40 to 65%. Over a 15-month period,
patients 55 years or older who had mood disorder evidenced a mortality rate
four times higher than expected, and coronary heart disease or stroke accounted
for 63% of the deaths. Depression may promote poor adherence to cardiac
rehabilitation and worse outcome. During the first year following MI,
depression is considered to be associated with a three- to fourfold increase in
subsequent cardiovascular morbidity and mortality. Depression in patients with
coronary artery disease is associated with more social problems, func-tional
impairment and increased health care utilization. Recent studies of erectile
dysfunction, cardiovascular disease and de-pression demonstrate that all three
conditions share many of the same risk factors.
Cancer
MDD occurs in 25% of patients with cancer at some time during the
illness. MDD should be assessed and treated as an independ-ent disorder. The
intense reaction in patients diagnosed with cancer may lead to dysphoria and
sadness without evolving a full syndrome of MDD. The consulting psychiatrist
must evalu-ate the patient’s response to chemotherapy, side effects of the
treatment, and medication interactions in the overall assessment of the
patient. Among patients with cancer, MDD is typically characterized by
heightened distress, impaired functioning and decreased capacity to adhere to
treatment. Treating comorbid MDD with psychotherapy or pharmacotherapy may
improve the overall outcome in patients with cancer and mitigate complica-tions
of MDD.
Chronic Fatigue Syndrome
Lifetime rates of MDD in patients with chronic fatigue syndrome range
from 46 to 75%. Comorbid anxiety and somatization dis-orders are also common in
patients with chronic fatigue. Ac-cording to the Centers for Disease Control
(CDC) criteria, the diagnosis of chronic fatigue syndrome is excluded in
patients whose symptoms meet criteria for a formal psychiatric disorder. such
as MDD or DD. Patients whose symptoms meet criteria for both a mood disorder
and chronic fatigue syndrome should be maximally treated for the mood disorder
with appropriate phar-macotherapy and cognitive–behavioral psychotherapy. The
etio-logical relationship between mood disorder and chronic fatigue syndrome is
unclear.
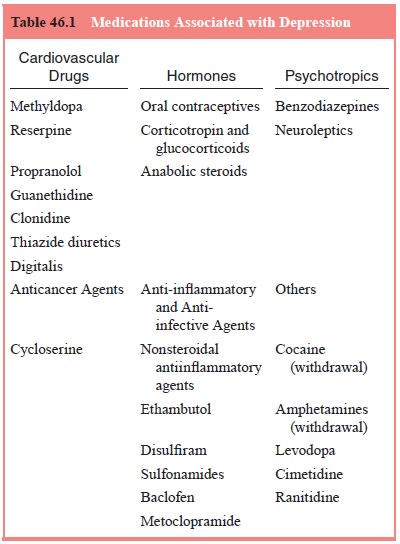
Depression Due to Medications
If MDD is judged to be a direct physiologic effect of a medica-tion,
then substance induced mood disorder is diagnosed. Medi-cations reported to cause
depression involve several drugs from the associated groups listed in Table
46.1.
Among antihypertensive treatment, beta-adrenergic blockers have been
studied regarding the risk of depression. No significant differences are found
between individuals treated with beta-blockers and those treated with other
antihyperten-sives regarding the propensity to develop depressive symp-toms.
Lethargy is the most common side effect reported. No significant depressive
complications are reported with calcium channel blockers or angiotensin
converting enzyme (ACE) inhibitors.
Hormonal treatments, such as corticosteroids and ana-bolic steroids, can
elicit depression, mania, or psychosis. Oral contraceptives require monitoring
regarding the possible pre-cipitation of depressive symptoms. Because patients
with seizure disorders and Parkinson’s disease are at high risk for concomitant
MDD, it is difficult to establish a link between anticonvulsant or
antiParkinsonian treatment and the precipitation of depression. Nevertheless,
patients require close monitoring and evaluation for evolution of depressive
symptomatology
Related Topics