Chapter: Essentials of Psychiatry: Mood Disorders: Depression
Depression: Pharmacotherapy and Other Somatic Treatment
Pharmacotherapy and Other Somatic Treatment
Treatment during the acute phase with medication is highly effi-cacious
in reducing signs and symptoms of MDD. Antidepressant medication has the most
specific effect on reduction of symptoms and is often associated with improved
psychosocial functioning. When symptoms of depression are mild to moderate, a course
of depression-specific psychotherapy without medicine may also be effective. If
symptoms of depression are moderate to severe, acute phase treatment with
medications is often indicated. A wide variety of antidepressant medications
have been documented as effective in moderate to severe MDD.
The range of treatments available in the USA has included the tricyclic
antidepressants, monoamine oxidase inhibitors (MAOIs), heterocyclic
antidepressants and SSRIs. In addition, antidepressants with both serotonergic
and noradrenergic ac-tivity or noradrenergic activity alone have become
available. Clearly, clinical trials comparing the efficacy of newer treatments
with standard tricyclic antidepressants have shown equal efficacy with
improvement in overall tolerance to side effects with newer treatments.
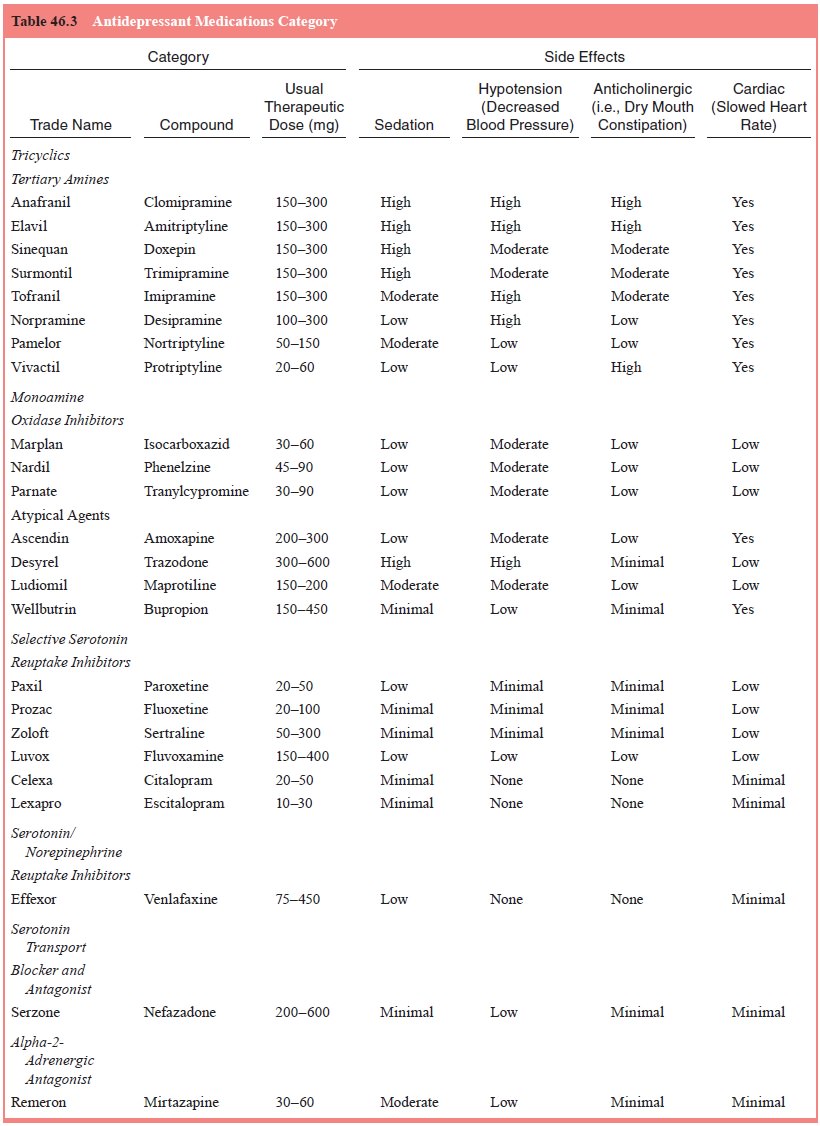
Antidepressant medications which are currently available for acute
treatment of MDD are listed in the associated table (Table 46.3).
Choice of treatment with a specific antidepressant treat-ment in a given
clinical situation is based on prior treatment response to medication,
consideration of potential side effects, history of response in first-degree
relatives to medicines, and the associated presence of cooccurring psychiatric
disorders that may lead to a more specific choice of antidepressant treat-ment.
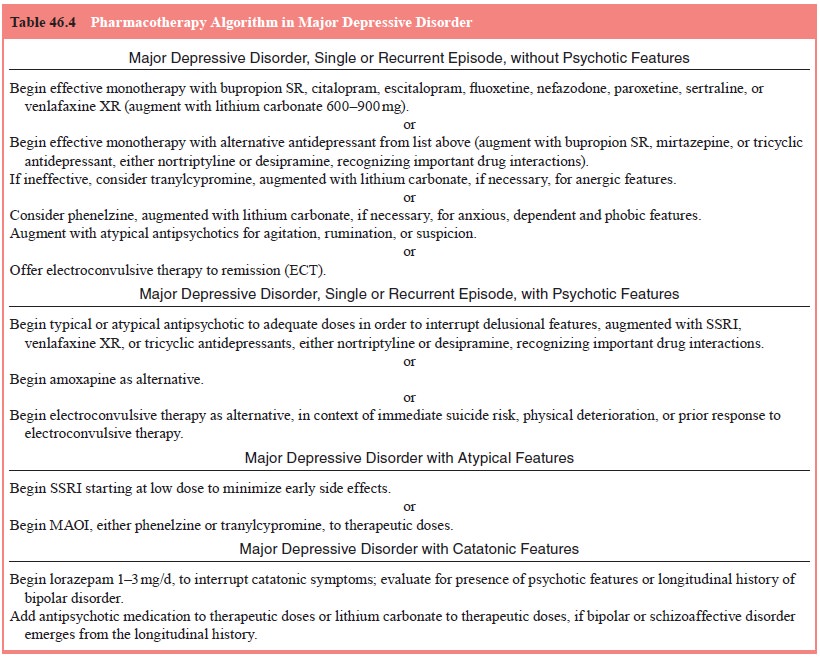
Table 46.4 illustrates an algorithm developed for pharma-cotherapy of MDD which
includes a staged trial of newer medi-cations (because of their superior
side-effect profiles) followed by treatments with older medicines available for
the treatment of MDD. The ultimate goal of pharmacotherapy is complete
remission of symptoms during a standard 6- to 12-week course of treatment.
Selective Serotonin Reuptake Inhibitors
The most commonly prescribed antidepressant medicines in the past 10
years are SSRIs. They are selectively active at se-rotonergic neurochemical
pathways and are effective in mild to moderate nonbipolar depression. They may
also be particularly effective in MDD with atypical features as well as DD.
Often these treatments are well tolerated and involve single daily dos-ing for
MDD. Because of selective serotonergic activity, these treatments have also
been demonstrated to be effective with cooccurring OCD, panic disorder,
generalized anxiety disorder, PTSD, premenstrual dysphoric disorder, bulimia
nervosa, so-cial anxiety disorder, as well as MDD. They tend to be reason-ably
well tolerated in individuals with comorbid medical con-ditions. There are
particular medication-specific interactions based on inhibition of cytochrome
P-450 liver enzyme systems which require attention if an individual is taking
other medica-tions for primary medical conditions or associated psychiatric
conditions. The currently available SSRIs in the USA include fluoxetine,
paroxetine, sertraline, fluvoxamine, citalopram and escitalopram.
Other Newer Antidepressants
In addition to SSRIs, greater attention has been brought to medi-cines with dual noradrenergic and serotonergic pathways includ-ing venlafaxine which has become available in both immediate release (IR) and extended release formulations. In addition, an alpha-2-adrenergic agonist, mirtazapine has become available, as well as a serotonin transport blocker and antagonist nefazodone. Recent concerns about hepatic complications associated with nefazodone has required liver function monitoring. A predomi-nantly noradrenergic and dopaminergic agonist, bupropion is also available in an immediate release and sustained release (SR) preparation. The newest dual acting antidepressant marketed in the USA is duloxetine.
Tricyclic Antidepressants in Individuals with Severe MDD Including Melancholic Features
Tricyclic antidepressants have been best studied in individuals with MDD
with melancholic features and with psychotic fea-tures. The combination of
typical antipsychotic pharmacother-apy in association with tricyclic
antidepressants has been rec-ommended. The side-effect profile of tricyclic
antidepressants has included moderate to severe sedation, anticholinergic
effects including constipation and cardiac effects which has made these
medicines less popular in typical primary care or psychiatric practice.
Nevertheless, the secondary amines which are metabo-lites of imipramine and
amitriptyline, specifically desipramine and nortriptyline, have continued to be
useful agents in more re-fractory depression.
Monoamine Oxidase Inhibitors
There continues to be a role for the use of MAOIs in patients with MDD
with atypical features. These agents particularly may be useful in intervention
in depressive episodes with atypical features, characterized by prominent mood
reactivity, reverse neurovegetative symptom patterns (i.e., overeating and
over-sleeping) and marked interpersonal rejection sensitivity. MAOIs continue
to have a significant role in treatment of comorbid panic disorder, social
phobia and agoraphobia if individuals are not responsive to SSRIs. The ongoing
prescription of phenelzine or tranylcypromine requires continued education of
the patient regarding standard food interactions involving tyramine as well as
specific drug–drug interactions involving sympathomimetic medications. These
cautions regarding diet and drug interaction makes MAO inhibitors less
attractive to primary care physicians and most psychiatrists. However, they
continue to be effective treatments which may be useful in depression with
atypical fea-tures as well as anergic bipolar depression.
Therapeutic Blood Levels
Although therapeutic blood level monitoring in the treatment of MDD may
have a role in future treatments, the only group of medicines where there has
been reliable assessment of blood lev-els are the tricyclic antidepressants.
Because tricyclic antidepres-sants have significant drug–drug interactions with
certain SSRIs there continues to be a need for therapeutic blood monitoring
particularly with nortriptyline and desipramine.
General Pharmacotherapy Recommendations
Increasingly, a trial of one class of antidepressants may be associ-ated
with incomplete response leading to a question of augment-ing a treatment with
another medicine versus switching from one medicine to another within the same
class or to a different class altogether. Augmentation strategies with other
medications, in-cluding adding lithium carbonate and other antidepressants,
particularly those with a different mechanism of action, atypical
antipsychotics, thyroid and stimulants, have been the focus of a number of
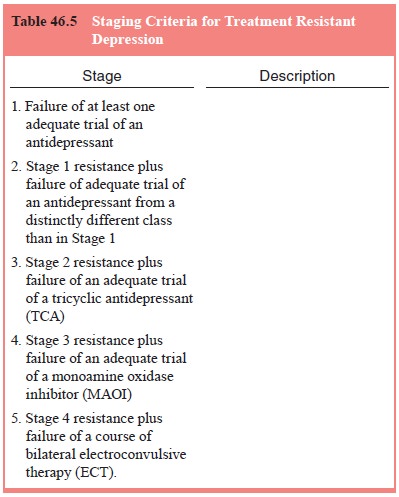
reviews of treatment resistance. A staging system for treatment resistant
depression (TRD) has been proposed and ranges from failure to respond to a
single agent (Stage 1) to failure of multiple treatments and electroconvulsive
therapy (Stage 5) as shown in Table 46.5.
Clinical Management
All of the antidepressant medications used in the treatment of MDD must
be prescribed in the context of an overall clinical
psychiatric relationship characterized by supportive interaction with
the patient and family and ongoing education about the nature of the disorder
and its treatment. Clinical management optimally involves careful monitoring of
symptoms using stand-ardized instruments and careful attention to side effects
of medi-cation in order to promote treatment adherence. Outpatient visits,
which may be scheduled weekly at the outset of treatment, and subsequently
biweekly encouragement and sustain collaborative treatment relationships. These
office consultations allow the psy-chiatrist to make dosage adjustments as
indicated, monitor side effects and measure clinical response to treatment.
For the majority of individuals with MDD, a course of 6 to 8 weeks of
acute treatment with weekly outpatient visits is indicated. Subsequent office
visits may be scheduled every 2 to 4 weeks during the continuation phase of
treatment. Appropri-ate adjustments of dose are determined by the psychiatrist
as indicated by best clinical judgments of medication effect. The dose of an
SSRI may be adjusted every 3 days on the basis of telephone contact and
follow-up visits may be scheduled every 7 to 10 days. Similarly, the adjustment
of dosing of tricyclic anti-depressants and MAOIs must be attended to carefully
in the first 2 to 3 weeks of treatment. Optimal dosing ranges of SSRIs,
tri-cyclics and MAOIs are noted in Table 46.3. Because of the early anxiety,
agitation and occasional insomnia associated with SS-RIs, somewhat lower doses
may be initiated early in the course before achieving the typical standard
therapeutic dose.
Incomplete response, which entails the failure to respond to acute
treatment with an antidepressant medication at 6 to 8 weeks, requires
reassessment of diagnosis and determination of adequacy of dosing. Ongoing
substance abuse, associated general medical condition or concurrent psychiatric
disorder may partially explain a lack of complete response. If substance
dependence is present, a full substance-free interval (preferablyweeks or
longer) with appropriate detoxification and rehabilita-tion may be indicated.
If a reassessment discloses an associated psychiatric disorder, then more
specific treatment of that associ-ated disorder, whether it be bipolar disorder
or concurrent post traumatic disorder, is necessary. If the reassessment
suggests an associated comorbid personality disorder, then appropriate and more
specialized psychotherapy may be necessary in order to achieve a complete
response to treatment. As indicated before, if the MDD has psychotic features,
then antipsychotic pharma-cotherapy to adequate doses must be initiated prior
to initiating a course of standard tricyclic antidepressants or a combined
se-rotonin norepinephrine uptake inhibitor such as venlafaxine. If MDD is
associated with severe personality disorder (e.g., bor-derline personality
disorder), then adjunctive psychotherapy and low dose antipsychotic medications
may be necessary. If the pa-tient has severe melancholic, delusional, or
catatonic features, a course of electroconvulsive therapy may be necessary to
achieve remission of symptoms.
There is also evidence that continuation of treatment be-yond 6 to 12
weeks may convert some partial responders to re-sponders if drug treatment is
increased to full doses. This time allows for evaluation of the role of focused
psychotherapy to ad-dress residual interpersonal disputes, loss or grief, or
ongoing social deficits. The associated augmentation strategies to stand-ard
treatments include lithium carbonate augmentation, tricyclic antidepressant
augmentation of SSRIs, thyroid hormone aug-mentation and bupropion augmentation
of SSRIs.
Electroconvulsive Therapy
Electroconvulsive therapy (ECT) remains an effective treat-ment in
patients with severe MDD and those individuals with psychotic MDD. Many
patients who have responded to electro-convulsive therapy do not respond to
pharmacotherapy. There is increased need for understanding the role of
maintenance electroconvulsive therapy in those individuals who respond to
electroconvulsive therapy because ongoing pharmacotherapy does not always
prevent recurrence of depression after ECT is successful. ECT can be
particularly useful in interrupting acute suicidality for those patients who
may require rapid resolution of symptoms. ECT may be indicated in older adults
when lack of self-care and weight loss may represent a greater risk. The most
common side effect associated with electroconvulsive therapy is amnesia for the
period of treatment. There is no consistent evidence to suggest chronic
cognitive or memory impairment as a result of ECT.
Other Somatic Treatments
Light therapy investigators have continued to demonstrate ben-efit in
individuals with seasonal MDD by providing greater than 2500 lux light therapy
for 1 to 2 hours/day. Many of these patients experience recurrent winter
depression in the context of a recur-rent MDD or bipolar II disorder. Bright
light exposure has been associated with favorable response within 4 to 7 days.
As with electroconvulsive therapy, light therapy is best prescribed by
specialists who have experience in its use and can appropriately evaluate the
indication for light therapy and monitor carefully the response to treatment.
Ongoing investigation of alternative brain stimulation techniques have
been the subject of recent investigation. The use of a powerful magnet to
provide transcranial magnetic stimula-tion has been the subject of several open
trials. It is not yet deter-mined whether the repetitive transcranial magnetic
stimulation demonstrates its effectiveness through reduction of inhibitory
neurotransmission or other mechanisms.
In addition, open clinical trials of vagus nerve stimula-tion (VNS)
which has been found to be effective in epilepsy has been the subject of
attention in refractory MDD. Several sites of investigation have begun to
reveal positive effects at 9 months using VNS implantation. This procedure
requires the implan-tation of a stimulating device in the chest with the
capacity to stimulate the vagus nerve at regular intervals through the course
of the day.
Related Topics