Chapter: Essentials of Psychiatry: Psychological Factors Affecting Medical Condition
Psychological Factors Affecting Medical Condition
Psychological Factors Affecting
Medical Condition
Definition
This
diagnostic category recognizes the variety of ways in which specific
psychological or behavioral factors can adversely affect medical illnesses.
Such factors may contribute to the initiation or the exacerbation of the
illness, interfere with treatment and reha-bilitation, or contribute to
morbidity and mortality. Psychological factors may themselves constitute risks
for medical diseases, or they may magnify the effects of nonpsychological risk
factors. The effects may be mediated directly at a pathophysiological level
(e.g., psychological stress inducing myocardial ischemia) or through the
patient’s behavior (e.g., noncompliance).
The
criteria in the Diagnostic and
Statistical Manual of Mental
Disorders, Fourth Edition (DSM-IV) includes situations in which psychological factors interfere
with medical treatment, pose health risks, or cause stress-related
pathophysiological changes. This diagnosis is structured in DSM-IV so that both
the psycho-logical factor and the general medical condition are to be speci-fied.
The psychological factor can be an Axis I or Axis II mental disorder (e.g.,
major depressive disorder aggravating coronary ar-tery disease), a
psychological symptom (e.g., anxiety exacerbating asthma), a personality trait
or coping style (e.g., type A behavior contributing to the development of
coronary artery disease), mal-adaptive health behaviors (e.g., unsafe sex in a
person with human immunodeficiency virus [HIV] infection), a stress-related
physi-ological response (e.g., tension headache), or other unspecified
psychological factors. The medical condition is noted on Axis III.
The
subject of psychological factors affecting medical con-dition (PFAMC) has
become the focus of intense research because of the illumination it may provide
of basic disease mechanisms (e.g., psychoneuroimmunology) and because of the
deep interest in improving both the outcomes and the efficiency of health care
delivery. In epidemiological studies, several psychiatric disorders increase
the likelihood of mortality especially depression, bipolar disorder,
schizophrenia, and alcohol abuse or dependence. Psy-chiatric disorders or
symptoms in patients with medical illness may increase their use of health care
services, particularly the length of costly hospital stays. Interest has been
further increased by intervention trials aimed at psychological factors or
disorders that have demonstrated improvements in medical outcomes and in
quality of life in patients with serious medical disorders.
It should
be evident that this diagnosis is not really a dis-crete diagnostic category
but rather a label for the interactive effects of psyche on soma. Mind–body
interactions have long been a focus of interest, both in health and in disease.
Psychiatric
illness
and medical disease frequently coexist. Psychiatrists and investigators of past
eras were misled by this frequent comor-bidity into premature conclusions that
the psychological factors were preeminent in the causation of the medical
disorders, and these were designated psychosomatic. A more modern approach has
been to recognize that all medical illnesses are potentially affected by many
different factors in the biological, psychologi-cal and social realms. The
earlier designation of certain disor-ders as psychosomatic (e.g., peptic ulcer
disease) overvalued the contribution of psychological factors to those
disorders and undervalued their contribution to other medical disorders (e.g.,
cancer). Furthermore, whereas labeling medical illnesses as psy-chosomatic drew
attention to the importance of mind–body in-teractions, it unfortunately and
falsely implied to many patients and physicians that the illness was basically
psychogenic, that the symptoms were not “real”, and that the illness was
somehow the patient’s fault.
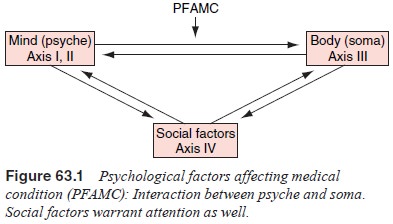
The
diagnosis of PFAMC focuses attention on one causal direction in the
interactions between psyche and soma, that is, the effects of psychological
factors on the medical condition (Figure 63.1). This represents a heuristic
simplification, high-lighting a particular process for further exploration,
understand-ing, and intervention. In most patients, there are effects in the
other direction as well (i.e., the effects of general medical illness on
psychological function). Furthermore, both mind and body in-teract with social
and environmental factors both dramatic (e.g., poverty, racism, war) and more
subtle (e.g., employment status, neighborhood), that affect the incidence and
outcome of medical illness. Diagnosing PFAMC may help psychiatrist and patient
ad-dress an important dimension of care, but the other “arrows” of Figure 63.1
often warrant attention too.
Related Topics