Chapter: Essentials of Psychiatry: Psychological Factors Affecting Medical Condition
Psychological Factors Affecting Medical Condition: Epidemiology and Comorbidity, Course
Epidemiology and Comorbidity
Because
this diagnosis describes a variety of possible interac-tions between the full
range of psychiatric disorders (as well as symptoms and behaviors) on the one
hand and the complete range of medical diseases on the other, it is impossible
to estimate over-all rates of prevalence or incidence. We can start, however,
by noting how frequently medical and psychiatric disorders coexist. Psychiatric
problems are common in medical patients, although the measured frequency
varies, depending on the criteria and method of measurement used. A reasonable
estimate is that 25 to 30% of medical outpatients and 40 to 50% of general
medi-cal inpatients have diagnosable psychiatric disorders (Table 63.1). Most
common in medical outpatients are depression, anxiety and substance abuse; medical
inpatients most often have cogni-
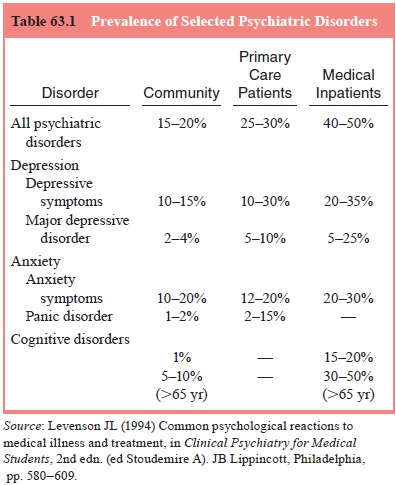
tive
impairment (delirium, dementia), depression and substance abuse. Depression,
both as a diagnosis and as a symptom, has been better studied in the medically
ill than any other psychiatric syndrome. Major depressive disorder occurs in 18
to 25% of pa-tients with serious coronary disease, in 25% of those with cancer,
and at three times the normal rate in diabetic patients. Individu-als
presenting with symptoms of chronic fatigue have a 50 to 75% lifetime
prevalence of major depression.
Nonpsychiatric
physicians under diagnose and under treat psychiatric disorders in the
medically ill. Medical disorders are also common in patients seen for mental
health treatment, and mental health specialists often under recognize the
presence and significance of coexisting medical disorders. Regardless of
whether the patient has come seeking medical care or men-tal health care,
medical and psychiatric problems are often both present. Such coincidence by
itself is not sufficient for the diag-nosis of PFAMC. In some cases, the
illnesses may coexist with little effect on each other; in other cases, the
effects of the medi-cal illness on the psychiatric condition may be more
important. The diagnosis of PFAMC in DSM-IV is reserved for patients in whom
psychological factors adversely affect a medical condition in a specifiable
way.
Course
Given the
wide range of psychiatric disorders and psychological factors that may affect
medical illness and the large number of different medical disorders that may be
influenced, there are no general rules about the course of the PFAMC
interaction. Psy-chological factors may have minor or major effects at a
particular point or throughout the course of a medical illness. We do know in
general that patients with medical disorders who also have significant
psychological symptoms have poorer outcomes and higher medical care costs than
those patients with the same med-ical disorders but without psychological
distress. A number of studies now document that psychological or psychiatric
problems (particularly cognitive disorder, depression and anxiety) in gen-eral
medical inpatients are associated with significant increases in length of
hospital stay. Psychosocial interventions have been able to improve outcomes in
medical illness, sometimes with an attendant savings in health care costs.
Related Topics