Nursing - Procedure and Recording of Temperature | 11th Nursing : Chapter 5 : Nursing - Health Assessment and Physical Examination
Chapter: 11th Nursing : Chapter 5 : Nursing - Health Assessment and Physical Examination
Procedure and Recording of Temperature
Procedure and Recording of Temperature
Body temperature is
its degree of heat. Normally the degree at which balance between heat
production and heat loss is maintained is called the “Normal Body Temperature”.
It is also called as “Normothermia or Euthermia”.
Factors affecting body temperature
1) Age, 2) Exercise,
3) Hormone level, circadian rhythm 5) Stress, 6) Environment, 7) Temperature
attraction, ever, 9) Hyperpyrexia, 10) Heat stroke, Hypothermia
1.
Age: Temperature regulation
is unstable until children reach
puberty. Older adults are sensitive to temperature extremes because of
deterioration in control mechanisms, reduced sweat gland activity, reduced
amounts of subcutaneous fat and reduced metabolism
2.
Exercise: Muscle activity causes increased metabolism by increasing carbohydrate and fat
breakdown. Any form
of exercise can increase heat production and the body temperature because of
increased metabolism.
3.
Hormone level: Women generally experience greater fluctuations in
body temperature than men. Hormonal variations during menstrual cycles cause
body temperature fluctuation.
Temperature changes occur in women during menopause
(cessation of menstruation).
4.
Circadianrhythm:Bodytemperature normally changes from 0.5º to 1ºC
during 24 hours period. The temperature is usually lowest between 1.00 AM and
4.00 AM
5.
Stress: Physical and emotional stress increases body temperature through
hormonal and neural stimulation. Those physiological changes increase
metabolism, which increases heat production.
6.
Environment:Environmentinfluences body temperature because of extensive
radiant and conductive heat loss.
7.
Temperature attraction: Changes in body temperature can be related to excess heat loss, minimal heat
production, minimal heat loss or any combination of these.
8.
Fever: Hyperpyrexia or fever occurs because heat loss mechanisms are
unable to keep pace with excess heat. Production, resulting in an abnormal rise
in body temperature.
9.
Hyperpyrexia: An elevated body temperature related to the body’s
inability to promote heat loss or reduce heat production is hyperthermia. Any
disease or trauma to the hypothalamus can impair heat loss mechanisms.
10.
Heat stroke: Prolonged exposure to the sum or high environmental
temperature can overwhelm the body’s heat loss mechanisms. Heat also depresses
hypothalamic function. These conditions cause heat stroke, a dangerous
emergency condition with a high mortality rate. Patients at risk for heat
stroke are the very young, very old, cardio vascular condition, diabetes and
alcoholics.
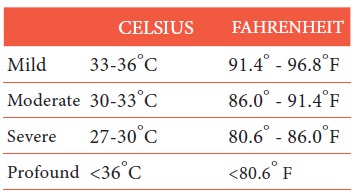
11. Hypothermia: Heat loss during prolonged
exposure to cold overwhelms the body ability to produce heat causing
hypothermia. Hypothermia is classified
as follows:
Sites for assessing temperature:
1) Oral
2) Rectal
3) Auxiliary
4) Groin
5) Ear (Tymphanic membrance)

The Mouth (oral Temperature)
This is a convenient, reliable and
commonly used method, but should not be used if the patient is;
a)
A child under 6 years of age
b)
Unconscious, mentally confused or very nervous condition
c)
Very weak, so that the mouth may full open
d)
Having breathing difficulty or frequent cough
e)
Having an injured of inflammed mouth.
Contra Indications
1)
Oral temperature: Temperature should also not be taken by mouth
soon after a hot drink (or) hot bath
2) Rectal: Rectal temperature is used
for very ill patients, for infants and children. The reading is a little higher
than oral when the temperature is taken by rectum
3)
The Axilla: This is convenient when the temperature cannot be
taken by mouth. It is less accurate and the reading will be a little lower than
when taking by mouth. The axilla must be dried and the thermometer is placed.
So that the bulb is in contact with both skin surfaces the arm should be held
close to the chest.
4)
Groin: This is a convenient site in children. The groin must be
wiped dry and the thigh well flexed over the abdomen and held there.
5) Ear: It is also a convinient site
for mentally disturbed patients. For assessment, digital thermometers are used.

Types of Thermometers
1)
Mercury thermometers (Clinical thermometer)
2)
Electronic thermometer
3)
Temporal artery thermometer
4)
Disposable thermometer
1.
Mercury thermometers (Clinical
thermometer):Clinicalthermometers are meant for clinical purposes. It is
developed for measuring the human body temperature. It is a long narrow glass
tube with a bulb containing mercury at the end.
The normal human body temperature is 37ºC. It can
fluctuate between the ranges 35ºC. The level of mercury tells our body
temperature in ºC. Since mercury is toxic element has been eliminated from
health care facilities because of the environmental hazards of mercury. When
you find a mercury – in – glass thermometer in the home

Teach the patient about safer temperature devices and
encourage the disposal of mercury products at appropriate neighbourhood
hazardous disposal locations.
2.
Electronic thermometer: The electronic thermometer consists of a rechargable battery – powered
display unit, a thin wire cord and a temperature – processing probe covered by
a disposable probe cover. Separate unbreakable probes are available
For oral and rectal use. You can also use the oral probe
for auxiliary temperature measurement. Electronic thermometers provide two
modes of operation; a 4-second predictive temperature and a 3-minute standard
temperature. A sound signals, and a … Readings appears on the display unit when
the Peak temperature readings has been measured.
3.
Temporal artery thermometer: Measures the temperature of the
superficial temporal artery. A handheld scanner with an infrared sensor tip
defects the temperature of Cetaceous blood flow by sweeping the sensor across
the forehead and just behind the ear. After scanning is complete, a reading
appears on the display unit. Temporal artery temperature is reliable
non-invasive measure of core temperature.

4.
Disposable thermometer: Single use (or) reusable chemical dot thermometers are thin strips of
plastic with dots on the surface that have been impregnated with temperature –
sensitive chemicals. The strips are sticker on the armpit and prevent slippage.
The dots change colour at different temperatures (within
60 seconds) as the chemicals in them respond to body heat. In the Celsius
version there are 50 dots, each representing a temperature increment of 0.1ºC,
over a range of 35.5 – 40.4ºC.

The Fahrenheit version has 45 dots with increments of
0.2ºF and range of 96-104.8ºF. Disposable thermometers are usually for oral
temperatures. You also use them at auxiliary with a placement time of minutes.
Chemical dot thermometers are useful for screening temperatures, especially in
infants and young children and patients who are incubated.
Purpose of Taking Temperature
1)
To aid in diagnosis or the patient’s condition
2) To find out the progress of the
patient.
Taking Temperature By Mouth
General Instructions
1)
Oral temperature should not be taken immediately after the
patient has had a hot or a cold drink or food.
2)
Oral temperature should not be taken for the following patients.
1.
Children below the age of five years
2.
Patients receiving oxygen
3.
Patients with nasal obstruction, dyspnoea or sore throat
4.
Patient who are delirious, unconscious and not cooperating, hysterical
5.
Restless or mentally ill
6.
Patients
with oral surgeries.
Recording temperature – oral Equipment
Tray Containing
1)
3 or 4 test tubes or bottles with antiseptic lotions (Savlon 2%)
and a little cotton underneath
2)
A glass tumbler with clean water and little cotton underneath
3)
A bowl containing a bit soapy white wipers
4)
A small piece of clean cloth
5)
A Kidney tray
6)
A Paper bag
7)
Watch with second hand
8)
Red lead pen
Procedure
1)
Explain the procedure and take the patients cooperation
2)
Let the patient be sitting or lying down
3)
Remove thermometer from the lotion, wash with clean water and dry
with clean piece of cloth form the bulb upwards to prevent bacteria from
setting down on the lower part which goes into the mouth of the patient.
4)
Shake down the mercury by 95ºF. Place the bulb of the
thermometer under the tongue and tell the patient not to bite the thermometer
but to hold it with his lips.
5)
Leave the thermometer in the mouth for 2 minutes (during this
time take his pulse and respiration)
6) Remove the thermometer, note the
temperature clean with the soapy wiper from above downwards towards the bulb(to
prevent bacteria from spreading all over the thermometer)
7)
Collect the dirty soapy water in the kidney tray and place the
dirty wiper in the paper bag.
8)
Replace thermometer in the test tube of bottle with the lotion
9)
Record the temperature in the chart
After care of the equipment
1)
Clean all the articles used
2)
Wash the thermometer with soap and cold water
3)
Keepthethermometerintheantiseptic lotion for 2 to minutes
4)
Reset the tray and keep it ready for the next use.
Conversion of Scales
To convert centigrade to
Fahrenheit, multiply by 9, divide by 5 and add 32.
To convert Fahrenheit to
centigrade, deduct 32, multiply by 5 and divide by 9
C = (F−32) x 5/9
F = 9/5×C+32
Abnormal temperature
1)
Subnormal-35oto36.1oC(95oto97oF)
2)
Collapse – below 35oC (95oF)
3)
Fever or pyrexia
Low pyrexia – 37.2oto 38.3oC (99oto
101oF)
Moderate Pyrexia – 38.3oto 39.4oC
(101oto 103oF)
High Pyrexia – 39.5o to 40.5oC (103oto
105oF)
Hyper Pyrexia – 40.5oC (105oF) and
above
Related Topics