Chapter: Medicine and surgery: Nervous system
Primary intracranial tumours - Tumours of the nervous system
Tumours of the nervous system
Primary intracranial tumours
Definition
Primary tumours arise from the neuronal or support cells of the central nervous system.
Incidence
Primary brain tumours account for only 2% of all tumours (although metastases are the most common intracranial tumour). The incidence appears to be rising, only partly due to increased detection.
Age
The age of presentation depends on the underlying histology. Overall, tumours peak around the age of 50–60 years, but most medulloblastomas and other embryonal tumours occur before the age of 20 years.
Aetiology/pathophysiology
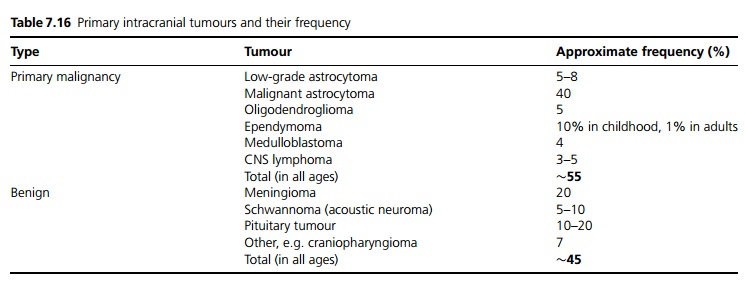
The only known risk factors for primary tumours are highdose radiation, e.g. in atomic bomb survivors, following radiation treatment for childhood leukaemia, and genetic factors, such as in neurofibromatosis (acoustic neuromas). Most tumours grow slowly and many malignant tumours probably arise from benign tumours (see Table 7.16).
Clinical features
Mass lesions within the skull produce signs and symptoms by three mechanisms:
· Direct effect of the mass causing compression or infiltration of the surrounding nervous tissue causes focal neurological signs. This may also occur secondary to surrounding oedema or arterial or venous compromise, i.e. a stroke. Headache with focal neurology is a typical presentation.
· Raised intracranial pressure (ICP) usually develops slowly, so does not normally cause the typical triad of headache, vomiting and papilloedema. However, brainstem, floor of the third ventricle and cerebellar lesions tend to present initially with raised ICP:
i. Distortion of the upper brain stem causes impaired consciousness.
ii. Compression of the medulla due to herniation (coning) causes a third nerve lesion (due to compression of the ipsilateral third nerve) and sixth nerve lesion (due to stretching of the contralateral sixth nerve), ipsilateral hemiparesis, impaired consciousness, respiratory depression, bradycardia and death.
· Partial or generalised tonic clonic seizures are characteristic of many cerebral mass lesions.
Investigations
CT scanning will detect over 95% of intracranial tumours. MRI scanning, angiography is used for surgical planning. Biopsy is required for histological diagnosis, although a radiological diagnosis may be sufficient. Stereotactic biopsy has a high diagnostic yield and lower morbidity and mortality than standard open biopsy.
Management
Surgical debulking may be performed. Complete resection of benign tumours is preferred; however, if close to vital structures, e.g. brainstem lesions, this is not always possible.
Radiotherapy is used postoperatively, for unresectable lesions or in patients unfit for surgery.
Cerebral oedema is treated with corticosteroids.
Chemotherapy is used for malignant astrocytoma, to try to prolong survival by a few months.
Seizures are treated with anticonvulsants.
Prognosis
Prognosis correlates with histologic type and grade, post-operative size, extent of the tumour and by the patient characteristics (age, performance status, and duration of symptoms).
Related Topics