Chapter: Obstetrics and Gynecology: Hirsutism and Virilization
Polycystic Ovary Syndrome
POLYCYSTIC OVARY SYNDROME
Polycystic ovary syndrome (PCOS) is the most commoncause of
androgen excess and hirsutism.
The etiology of this disorder is
unknown. Some cases appear to result from a genetic predisposition, whereas
others seem to result from obesity or other causes of LH excess.
Symptoms
of PCOS include oligomenorrhea or amenorrhea, acne, hirsutism, and infertility.
The disorder is characterizedby chronic anovulation
or extended periods of infrequent ovulation (oligo-ovulation). It is a syndrome
primarily defined by excess androgen. The definition of PCOS has varied in the
past, resulting in the National Institutes of Health (NIH)-convening consensus
conferences in 1990 and 2000. In 2003 the Rotterdam consensus workshop
developed a more encompassing definition of PCOS. To establish the diagnosis,
the patient should have two of the following criteria:
Oligo-ovulation or anovulation
usually marked by irreg-ular menstrual cyclesBiochemical or clinical evidence
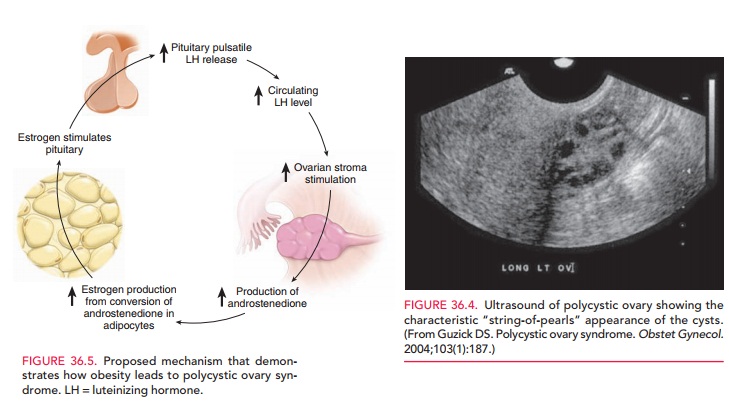
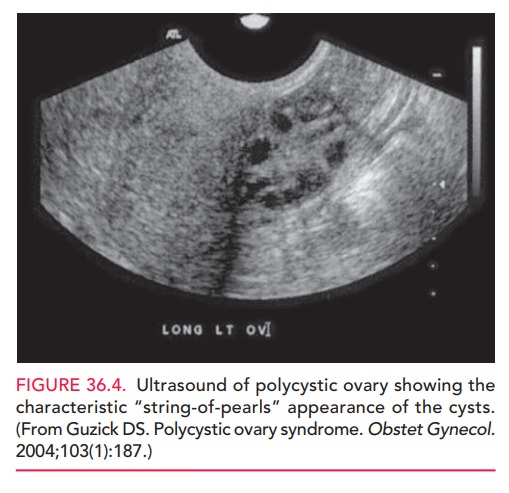
of hyperandrogenismPolycystic appearing ovaries on ultrasound (Fig. 36.4)
It is also important to rule out
other endocrine disorders that can mimic PCOS, such as congenital adrenal
hyper-plasia, Cushing syndrome, and hyperprolactinemia.
In many
women with PCOS, obesity seems to be the com-mon factor (seen in 50% of
patients), and the acquisition of body fat coincides with the onset of PCOS. In fact,
Stein andLeventhal first described PCOS as women with hirsutism, irregular
cycles, and obesity. (PCOS was originally called Stein-Leventhal syndrome.)
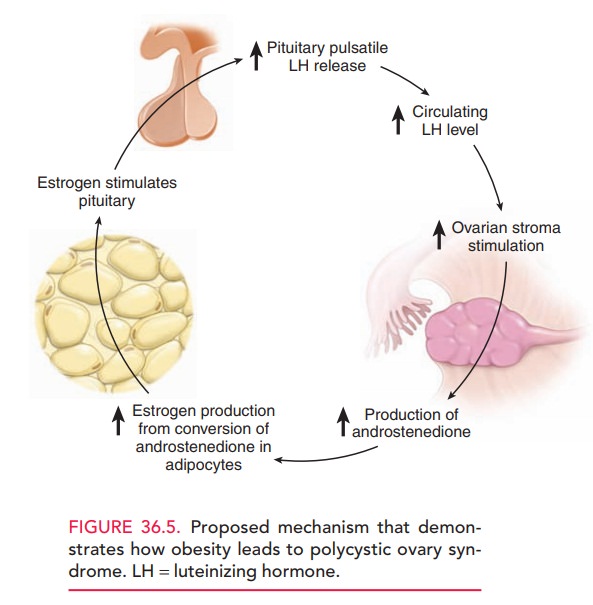
PCOS is related to obesity by the following mechanism: LH stimulates the
theca-lutein cells to increase androstenedione production. Andro-stenedione
undergoes aromatization to estrone within adipocytes. Although estrone is a
weak estrogen, it has a positive-feedback action or stimulating effect on the
pitu-itary secretion of LH. LH secretion is, therefore, stimu-lated by
increased estrogen. With increasing obesity comes increased conversion of
androstenedione to estrone. With the increased rise in androstenedione, there
is coincident increased testosterone production, which causes acne and
hirsutism (Fig. 36.5).
Hormonal
studies in women with PCOS show the follow-ing: (1) increased LH:FSH
(follicle-stimulating hormone) ratio, (2) estrone in greater concentration than
estradiol, androstenedione at the upper limits of normal or in-creased, and (4)
testosterone at the upper limits of normal or slightly increased.
Therefore, PCOS can be viewed as one of excess androgen and excess estrogen. The unopposed long-term elevated estrogen levels that characterize PCOS increases the risk of abnormal uterine bleeding, endometrial hyperplasia, and, in some cases, the development of endometrial carcinoma.
The typical woman with PCOS has
many of the signs of metabolic syndrome
(Syndrome X). Approximately 40% of patients with PCOS have impaired glucose
toler-ance, and 8% have overt type 2 diabetes mellitus. These patients should
be screened for diabetes. Classic lipid abnormalities include elevated
triglyceride levels, low high-density lipoprotein (HDL) levels, and elevated
low-density lipoprotein (LDL) levels. Hypertension is also common in
individuals with this condition. The combina-tion of the preceding
abnormalities potentially increases the risk of cardiovascular disease.
Acanthosis
nigricans has also been found in a signif-icant percentage of
these patients. The HAIR-AN syn-drome (hyperandrogenism,
insulin resistance, acanthosis nigricans) constitutes a defined subgroup of patients withPCOS.
Administration of the insulin-sensitizing agent metformin in these patients
also reduces androgen and insulin levels.
PCOS is a
functional disorder whose treatment should be targeted to interrupt the
disorder’s positive-feedback cycle.
The most common therapy for PCOS
is the administra-tion of oral contraceptives, which suppresses pituitary LH
The ovarian
contri-bution to the total androgen pool is thereby decreased. Acne clears, new
hair growth is prevented, and there is decreased androgenic stimulation of
existing hair follicles. By preventing estrogen excess, oral contraceptives
also prevent endometrial hyperplasia, and women have cyclic, predictable,
withdrawal bleeding episodes.
If a
woman with PCOS wishes to conceive, oral contracep-tive therapy is not a
suitable choice. If the patient is obese,
aweight-reduction diet designed to restore the patient to a normal weight
should be encouraged. With body weight
In some
women, ovulation induc-tion with clomiphene citrate is needed and is
facilitated by weight reduction. Insulin sensitizers (metformin) alone or with
clomiphene citrate may be used to reduce insulin resis-tance, control weight,
and facilitate ovulation.
Hyperthecosis is a more severe form of PCOS.In cases
ofhyperthecosis, androstenedione production may be so great that testosterone
reaches concentrations that cause viriliza-tion. Women with this condition may
exhibit temporal balding, clitoral enlargement, deepening of the voice, and
remodeling at the limb–shoulder girdle. Hyperthecosis is often refractory to
oral contraceptive suppression. It is also more difficult to successfully
induce ovulation in women with this condition.
Related Topics