Chapter: Biology of Disease: Pathogens and Virulence
Pathogens and Virulence: Introduction
PATHOGENS AND VIRULENCE
INTRODUCTION
The body is exposed to many pathogenic microorganisms
and multicellular parasites. Most microorganisms found associated with the body
are harmless and live as commensals or symbionts but others cause disease and
are known as pathogens. Infection, from the Latin ‘inficere’
(to put in), is the successful persistence and/or multiplication of the
pathogen on or within the host. In this respect, pathogenesis may be defined as the molecular and biochemical
mechanisms that allow pathogens to cause diseases. Mummies preserved in ancient
Egypt and elsewhere display evidence that infectious diseases have always been
a threat. The emergence of new pathogens and the development of resistance to
current treatments for existing pathogens means that infectious diseases will
probably always be with us.
Many antibiotic drugs are available to treat
infectious diseases and, in many cases, will effect a cure. It is, however,
possible for them to exacerbate the problem since the drug can remove
commensals allowing antibiotic resistant pathogens to flourish. Also, an
adequate immune response is often necessary, since drugs alone may fail to
eliminate the infection. Thus all pathogens must overcome the defense systems
present in their hosts .
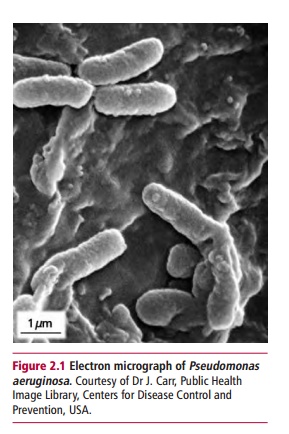
Some pathogens regularly cause diseases while others
do not. For example, Pseudomonas
aeruginosa (Figure 2.1) can cause
overwhelming disease inpatients whose defense systems are compromized but not
in those with intact defenses. It is likely that any microorganism with the
ability to live in or on humans will sometimes become an opportunistic pathogen especially if the balance between the usual
microorganisms present and the immune system is disturbed. Thus bacteria which
are normally harmless, but which are opportunistic pathogens, can cause
infections under certain conditions. For example, wounds can become badly
infected with bacteria that normally exist on the skin, and bacteria that
normally live in the gut can cause serious infections if peritonitis allows the
gut contents to enter the peritoneum. In general, these infections are not
transferable to other healthy humans.
The success of pathogenic microorganisms depends on
their ability to colonize host tissues and to counter the host’s defense
mechanisms. Virulence is measured by the infective
dose and the severity of the disease caused. For example, as few as 10 to
100 Shigella dysenteriae cells can
cause shigellosis but more than 10 000 cells are needed of the less virulent
salmonella or cholera bacteria. True pathogens are equipped with a range of virulence factors. The strains of some
bacterial species, such as pathogenic forms of Escherichia coli (Figure 2.2)
can produce different virulence factors that cause, for example, diarrhea,
urinary tract infections or sepsis. Other strains, however, do not produce
virulence factors or do so to a lesser extent and are therefore not pathogenic,
except when they infect an immunocompromized host.

A pathogen must be transmitted from a source to the
patient. Direct contact between hosts is the most obvious form of transmission
but coughs and sneezes (aerosols), food, water and arthropod vectors are all
used by various pathogens. The long-term survival of pathogenic microorganisms
also depends on maintaining their infectivity during transmission from host to
host. Diseases that are transmitted from animals to humans are called zoonoses, while humans who harbor a
pathogen but are asymptomatic arecalled carriers.
Related Topics