Chapter: Essentials of Psychiatry: Obsessive-Compulsive Disorder
ObsessiveŌĆōCompulsive Disorder Versus Other Disorders
ObsessiveŌĆōCompulsive Disorder Versus Other Anxiety
Disorders
Both OCD and the other anxiety disorders are characterized by the use of
avoidance to manage anxiety. However, OCD is distin-guished from these
disorders by the presence of compulsions. For OCD patients with preoccupying
fears or worries but no rituals, several other features may be useful in establishing
the diagnosis of OCD. In social phobia and specific phobia, fears are
circum-scribed and related to specific triggers (in specific phobia) or so-cial
situations (in social phobia). Although circumscribed situa-tions may initially
trigger obsessions and compulsions in OCD, triggers in OCD become more
generalized over time, unlike the triggers in social and specific phobias, in
which the evoking situ-ations remain circumscribed.
As many as 60% of people with OCD experience full-blown panic symptoms.
However, unlike panic disorder, in which panic attacks occur spontaneously,
panic symptoms occur in OCD only during exposure to specific feared triggers
such as contaminated objects. The worries that are present in generalized
anxiety dis-order (GAD) are more ego syntonic and involve an exaggeration of
ordinary concerns, whereas the obsessional thinking of OCD is more intrusive,
is limited to a specific set of concerns (e.g., contamination, blasphemy), and
usually has an irrational, sense-less, or unreasonable quality. Also, whereas
the worry of GAD is considered primarily thoughtlike in nature, obsessional
symp-toms may consist of thoughts, impulses, or images.
ObsessiveŌĆōCompulsive Disorder Versus Psychotic Disorders
One question is how to differentiate OCD from psychotic disorders such
as schizophrenia and delusional disorder. An-other question is how to
distinguish OCD with insight from OCD without insight (delusional OCD). One
distinguishing feature between OCD and the psychotic disorders is that the latter
are not characterized by prominent ritualistic behaviors. If compulsions are
present in a patient with prominent psy-chotic symptoms, the possibility of a
comorbid OCD diagnosis should be considered. Furthermore, although
schizophrenia may be characterized by obsessional thinking, other
character-istic features of the disorder, such as prominent hallucinations or
thought disorder, are also present. With regard to delusional disorder,
paranoid and grandiose concerns are generally not considered to fall under the
OCD rubric. However, some other types of delusional disorder, such as the
somatic and jealous types, seem to bear a close resemblance to OCD and are not
always easily distinguished from it. It will be interesting to see whether
future research indicates that certain types of so-matic delusional disorder
(e.g., the delusional variant of hypo-chondriasis) and the jealous type of
delusional disorder (also referred to as pathological jealousy) are actually
variants of OCD.
The second issue noted above ŌĆō how to distinguish OCD with insight from
OCD without insight ŌĆō is complex. As previ-ously discussed, insight in OCD is
increasingly being recognized as spanning a spectrum from good to poor to
absent. Both clini-cal observations and research findings indicate that some
indi-viduals hold their obsessional concerns with delusional intensity and
believe that their concerns are reasonable. In DSM-IV, delu-sional OCD may be
double-coded as both OCD and delusional disorder or as both OCD and psychotic
disorder not otherwise specified, in other words, patients with delusional OCD
would receive both diagnoses. This double coding reflects the fact that it is
unclear whether OCD with insight and OCD without insight constitute the same or
different disorders. Further research using validated scales to assess insight
in OCD is needed to shed light on this question.
ObsessiveŌĆōCompulsive Disorder Versus Impulse Control Disorders
Differential diagnosis questions have been raised with regard to
kleptomania, trichotillomania, pathological gambling and other disorders
involving impulsive behaviors. Several features have been said to distinguish
these disorders from OCD. For ex-ample, compulsions ŌĆō unlike behaviors of the
impulse control disorders ŌĆō generally have no gratifying element, although they
do diminish anxiety. In addition, the affective state that drives the behaviors
associated with these disorders may differ. In OCD, fear is frequently the
underlying drive that leads to com-pulsions, which, in turn, decrease anxiety.
In the impulse control disorders, patients frequently describe heightened
tension, but not fear, preceding an impulsive behavior. However, OCD and the
impulse control disorders have some features in common. Re-search is ongoing to
explore the relationship between OCD and the impulse control disorders by
examining similarities and dif-ferences in treatment response, biological
markers and familial transmission.
ObsessiveŌĆōCompulsive Disorder Versus TouretteŌĆÖs Disorder
Complex motor tics of TouretteŌĆÖs disorder may be difficult to
distinguish from OCD compulsions. Both tics and compulsions are preceded by an
intrusive urge and are followed by feelings of relief. However, OCD compulsions
are usually preceded by both anxiety and obsessional concerns, whereas, in
TouretteŌĆÖs disorder, the urge to perform a tic is not preceded by an
obses-sional fear. This distinction breaks down to some extent when considering
the ŌĆ£just rightŌĆØ perceptions of some patients with OCD. The ŌĆ£just rightŌĆØ
perception refers to the need to perform a certain motor action, such as
touching, tapping, checking, order-ing, arranging, or counting, until it feels
right. Determining when an action has been performed enough or perfectly may
depend on tactile, visual, or auditory perceptions. In a study of patients with
TouretteŌĆÖs disorder and OCD symptoms, most patients could distinguish between
the mental urge to do something repeatedly until it felt right and a physical
urge to perform a motor tic. How-ever, it is sometimes difficult for
psychiatrists to distinguish be-tween complex tics and compulsions, especially
when a patient has both disorders.
ObsessiveŌĆōCompulsive Disorder Versus Hypochondriasis
Fears of illness that occur in OCD, referred to as somatic obses-sions,
may be difficult to distinguish from hypochondriasis. Usu-ally, however,
patients with somatic obsessions have other cur-rent or past classic OCD
obsessions unrelated to illness concerns. Patients with OCD also often engage
in classic OCD rituals, such as checking or reassurance seeking, in an attempt
to diminish their illness concerns. Unlike patients with OCD, patients with
hypochondriasis experience somatic and visceral sensations. Although insight
and resistance have been used to distinguish OCD from hypochondriasis, with the
concern in hypochondria-sis being said to be egosyntonic (realistic and totally
justified) and that of OCD to be egodystonic (unacceptable and undesirable
thoughts, actions, or both), studies have demonstrated a range of insight in
OCD. Attempting to differentiate these disorders by degree of insight or
egosyntonicity may therefore be of limited usefulness.
ObsessiveŌĆōCompulsive Disorder Versus Body Dysmorphic Disorder
Body dysmorphic disorder (BDD), a preoccupation with an im-agined or
slight defect in appearance (e.g., thinning hair, facial scarring, or a large
nose), has many similarities to OCD (Phillips, 1991). Patients with BDD
experience obsessional thinking about the supposed defect and usually engage in
associated repetitive ritualistic behaviors, such as mirror checking and
reassurance seeking. Preliminary evidence suggests that BDD also appears
similar to OCD in terms of age of onset, course of illness and other variables.
Nonetheless, emerging data suggest that there are some important differences
between the two disorders, and they are currently classified separately in
DSM-IV. Insight, for example, is more frequently impaired in BDD than in OCD.
If the content of a patientŌĆÖs obsessions involves a concern about a supposed
defect in appearance, BDD, rather than OCD, is the diagnosis that should be
given.
ObsessiveŌĆōCompulsive Disorder Versus ObsessiveŌĆōCompulsive Personality Disorder
ObsessiveŌĆōcompulsive personality disorder is a lifelong mala-daptive
personality style characterized by perfectionism, exces-sive attention to
detail, indecisiveness, rigidity, excessive devo-tion to work, restricted
affect, lack of generosity and hoarding. OCD and OCPD have historically been
considered variants of the same disorder on a continuum of severity, with OCD
viewed as the more severe manifestation of illness. Contrary to this notion,
studies using structured interviews to establish diagnosis have found that not
all patients with OCD also have OCPD. One rea-son for the perception that these
disorders are linked lies in the frequency of several OCPD traits in patients
with OCD. In one study, the majority of 114 patients with OCD had perfectionism
and indecisiveness (82 and 70, respectively). In contrast, other OCPD traits,
such as restricted affect, excessive devotion to work and rigidity, were seen
infrequently.
Although perfectionism and indecisiveness are relatively common traits
in patients with OCD, the distinction between OCD and OCPD is important, and
several guidelines may be useful in distinguishing them. Unlike OCPD, OCD is
character-ized by distressing, time-consuming egodystonic obsessions and
repetitive rituals aimed at diminishing the distress engendered by obsessional
thinking. One of the hallmarks that traditionally has been used to distinguish
OCD from OCPD is that, in con-trast, OCPD features are considered egosyntonic.
In addition, as previously noted, the traits of restricted affect, excessive
devo-tion to work and rigidity are generally characteristic of OCPD but not
OCD. Although useful, these guidelines are not absolute, and some patients defy
easy categorization. Some patients, for example, spend hours each day engaged
in egosyntonic behav-iors such as excessive cleaning; such patients may seek
treatment not because they are disturbed by their behaviors but because the
behaviors cause problems in functioning or family friction. It is unclear
whether some of these patients should be diagnosed with OCPD or subthreshold
OCD.
ObsessiveŌĆōCompulsive Spectrum Disorders
Certain disorders other than OCD, such as BDD, hypochondria-sis, and
eating disorders, are characterized by obsessional think-ing and/or ritualistic
behaviors. On the basis of these apparent similarities with OCD, the concept of
OCD spectrum disorders has been developed. They have been defined as disorders
that share features with OCD (Hollander, 1993) and are posited to have
ŌĆ£spectrum membershipŌĆØ on the basis of their similarities with OCD across
multiple domains. These domains include not only symptoms but also treatment
response, comorbidity, joint familial loading, sex ratio, age at onset, course,
premorbid per-sonality characteristics and presumed cause. Cause is inferred
from characteristics such as neurological deficits, response to bi-ological challenges,
biochemical indices, brain imaging patterns (functional and anatomical) and
epidemiological risk factors. It is worth noting that there are currently no
operational criteria for what constitutes an OCD spectrum disorder; for
example, in which of the preceding domains must similarities be documented, and
how similar in each domain must the disorder be to OCD?
Disorders postulated to be OCD spectrum disorders in-clude BDD,
hypochondriasis, eating disorders, ŌĆ£groomingŌĆØ dis-orders such as nail biting
and trichotillomania, and the impulse
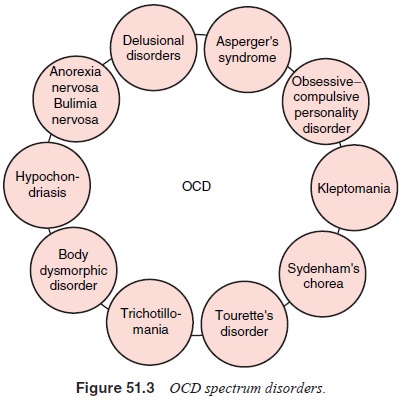
disorders
(see Figure 51.3). Of interest is a recent study investi-gating the frequency
of these disorders in first-degree relatives of people with OCD. BDD,
hypochondriasis, any eating disorder (although not anorexia or bulimia
individually) and grooming disorders (but not the impulse control disorders)
were found more frequently in probands with OCD than in general population
con-trols. In addition, BDD and grooming disorders (although not the other disorders)
were significantly more common in the first-degree relatives of OCD probands
than in relatives of controls (Bienvenu et al., 2000). This finding suggests
that certain of the proposed OCD spectrum disorders may have a familial link to
OCD. The relationship of these disorders with OCD is an area in which exciting
research will be conducted in coming years.
Related Topics