Chapter: Essentials of Psychiatry: Obsessive-Compulsive Disorder
Obsessive-Compulsive Disorder: Augmentation Strategies
Augmentation Strategies
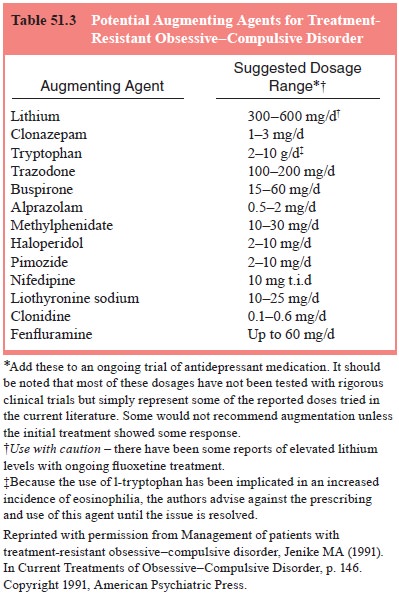
If a patient has had only a partial response to an antiobsessional agent
of adequate dose and duration, the next question is whether to change the SRI
or add an augmenting agent. Current clinical practice suggests that if there is
no response at all to an SRI, it may be best to change to another SRI. However,
if there has been some response to treatment, an augmentation trial of at least
2 to 8 weeks may be warranted. No augmentation agent has been firmly
established as efficacious. Many questions about augmen-tation remain
unanswered, including the optimal duration of aug-mentation, comparative
efficacy of different agents, predictors of response and mechanism of action.
Nonetheless, these agents do help some patients significantly, and thus their
systematic use should be considered (see Table 51.3).
In patients with severe symptoms or comorbid psycho-sis or tic disorder,
pimozide 1 to 3 mg/day, haldol 2 to 10 mg/ day, and other neuroleptic agents
(risperdone 2–8 mg/day and olanzapine 2.5–10 mg/day) have been used with some
success.
However, the use of a neuroleptic agent should be considered carefully
in light of the risk of extrpyramidal symptoms and side effects such as weight
gain, lethargy and tardive dyski-nesia. Thus, when a neuroleptic drug is used,
target symptoms should be established before beginning treatment, and the
med-ication discontinued within several months if target symptoms do not
improve.
The use of lithium (300–600 mg/day) and buspirone (up to 60 mg/day) as
augmentation agents has also been explored. Both agents looked promising in
open trials but failed to be effective in more systematic trials. Augmentation
with fenfluramine (up to 60 mg/day), clonazepam (up to 5 mg/day), clonidine
(0.1–0.6 mg/day) and trazodone (100–200 mg/day), as well as the combination of
clomipramine with any of the SSRIs, has had anecdotal success but has not been
evaluated in methodologically rigorous studies. Some potential augmenting
agents and their dosage ranges are presented in Table 51.3.
Behavioral Therapy
Behavioral therapy is effective for OCD both as a primary treat-ment and
as an augmentation agent. This form of therapy is based on the principle of
exposure and response prevention. The patient is asked to endure, in a
graduated manner, the anxiety that a specific obsessional fear provokes while
refraining from compulsions that allay that anxiety. The principles behind the
ef-ficacy of treatment are explained to the patient in the following way.
Although compulsions, either covert or overt, usually im-mediately relieve
anxiety, this is only a short-term solution; the anxiety will ultimately
return, requiring the performance of an-other compulsion. However, if the
patient resists the anxiety and urge to ritualize, the anxiety will eventually
decrease on its own (i.e., habituation will occur), and the need to perform the
ritual will eventually disappear. Thus, behavioral therapy helps the pa-tient
habituate to the anxiety and extinguish the compulsions.
Compulsions, especially overt behaviors like washing rituals, are more
successfully treated by behavioral therapy than are obsessions alone or covert
rituals like mental checking. This is because covert rituals are physically
harder to resist than are rituals like handwashing and checking a door. In fact
washing rituals are the most amenable to behavioral treatment, followed by
checking rituals and then mental rituals.
For rituals that do not constitute overt behaviors, tech-niques other
than exposure and response prevention have been used in conjunction with
exposure and response prevention. These approaches include imaginal flooding
and thought stop-ping. In imaginal flooding, the anxiety provoked by the
obses-sions is evoked by continually repeating the thought, often with the help
of a continuous-loop tape or the reading of a “script” composed by the patient
and therapist, until the thought no longer provokes anxiety. In thought
stopping, an compulsive mental rit-ual (e.g., continually repeating a short
prayer in one’s head) is stopped by simply shouting, making a loud noise, or
snapping a rubber band on the wrist in an attempt to interrupt the thought.
In the early stages of treatment, a behavioral assessment is performed.
During this assessment, the content, frequency, dura-tion, amount of
interference and distress, and attempts to resist or ignore the obsessions and
compulsions are catalogued. An at-tempt is made to clarify the types of
symptoms, any triggers that bring on the obsessions and compulsions, and the
amount and type of avoidance used to deal with the symptoms. For instance, in
the clinical vignette described later, the fact that Ms Z stopped preparing meals
to deal with her obsessional concerns about con-tamination was carefully
documented. The patient, usually with the help of a therapist, then develops a
hierarchy of situations ac-cording to the amount of anxiety they provoke.
During treatment, patients gradually engage in the anxiety-provoking situations
in-cluded in their hierarchy without performing anxiety-reducing rituals.
Behavioral therapy can be used with patients of any age and has been
used in young children, often with the help of a parent as a cotherapist.
However, systematic trials of behavioral treatment in children have not been
performed. More recently, behavioral therapy in a group setting has been
explored and found as effective as, and perhaps even more effective than,
indi-vidual behavioral treatment. The group seems to act as a catalyst for
change by promoting group cohesion, support and encour-agement. Groups can
include patients with different symptoms, though each has a personalized
hierarchy, so that one patient can encourage another. Van Noppen and associates
(1991) included family members in groups because families are often affected by
the patient’s rituals and often function as unwilling participants in rituals.
As members of the group, family members not only gain knowledge and
understanding about OCD but can be co-therapists at home for homework
assignments.
Despite its efficacy, behavioral therapy has limitations. To begin with, about 15 to 25% of patients refuse to engage in behav-ioral treatment initially or drop out early in treatment because it is so anxiety-provoking. Behavioral treatment fails in another 25% of patients for a variety of other reasons, including concomitant depression; the use of central nervous system depressants, which may inhibit the ability to habituate to anxiety; lack of insight; poor compliance with homework, resulting in inadequate expo-sure; and poor compliance on the part of the therapist in enforc-ing the behavioral paradigm. Thus, overall, 50 to 70% of patients are helped by this form of therapy.
One of the issues that has emerged in treating OCD with CBT is the lack
of trained therapists and the cost of repeated indi-vidual exposure sessions.
Thus, in addition to developing group treatments which allow therapists to
treat a number of patients simultaneously, researchers have begun to develop
computer-guided behavior therapy. Several recent reports have shown that while
this modality is not as effective as individual behavior therapy, it does allow
for significant improvement in symptoms over a control condition like
relaxation therapy.
Behavior therapy can be used as the sole treatment of OCD, particularly
with patients whose contamination fears or somatic obsessions make them
resistant to taking medications. Behavioral treatment is also a powerful
adjunct to pharmaco-therapy. Some research appears to indicate that combined
treat-ment may be more effective than pharmacotherapy or behavio-ral therapy
alone, although these findings are still preliminary. Some studies have even
suggested that adding pharmacotherapy to behavior therapy may be particularly
helpful in reducing ob-sessions while compulsions respond to behavior therapy.
From aclinical perspective, it may be useful to have patients begin treat-ment
with medication to reduce the intensity of their symptoms or comorbid
depressive symptoms if present; patients may then be more amenable to
experiencing the anxiety that will be evoked by the behavioral challenges they
perform.
Work by Baxter and colleagues (1992) has illustrated some interesting
correlations between treatment response and changes in neuroanatomy and
neurophysiology. Positron emission tomog-raphy scans with 18F-fluorodeoxyglucose were
performed on all patients before and after treatment. Compared with
nonrespond-ers and control subjects, responders in both the medication and the
behavioral treatment groups showed a decrease in activity in the right head of
the caudate nucleus. This finding seems to sup-port the notion that both forms
of treatment bring about similar changes in neurophysiology which lead to
improvement in symp-toms. These results also provide important theoretical
links with the serotonin hypothesis described earlier, as basal ganglion
structures like the caudate nucleus have been postulated to mediate serotonin
function.
Psychotherapy
The use of psychotherapeutic techniques of either a psychoana-lytic or a
supportive nature has not been proved successful in treating the specific
obsessions and compulsions that are a hall-mark of OCD. However, the more
characterological aspects that are part of obsessive–compulsive personality
disorder may be helped by a more psychoanalytically oriented approach. As noted
earlier, the defense mechanisms of reaction formation, isolation and undoing,
as well as a pervasive sense of doubt and need to be in control, are hallmarks
of the obsessive–compulsive char-acter. Salzman (1983) and MacKinnon and
Michels (1971) have written elegantly on how to approach the maladaptive
aspects of this character style in therapy. In essence, the patient must be
encouraged to take risks and learn to feel comfortable with, or at least less
anxious about, making mistakes and to accept anxiety as a natural and normal
part of human experience. Techniques for meeting such goals in treatment may
include the psychiatrist’s being relatively active in therapy to ensure that
the patient focuses on the present rather than getting lost in perfectly
recounting the past, as well as the psychiatrist’s being willing to take risks
and present herself or himself as less than perfect.
Neurosurgery
Occasionally, even after receiving adequate pharmacotherapy (including
augmentation), adequate behavioral therapy, and a combination of behavioral
therapy and pharmacotherapy, pa-tients may still experience intractable OCD
symptoms. Such patients may be candidates for neurosurgery. Although criteria
for who should receive neurosurgery vary, it has been suggested that failure to
respond to at least 5 years of systematic treatment is a reasonable criterion.
Frequently used criteria are the follow-ing: a minimum of two adequate
medication trials with augmen-tation plus adequate behavioral therapy in the
absence of severe personality disorder.
The procedures that have been most successful inter-rupt tracts involved
in the serotonin system. The surgical pro-cedures used – anterior capsulotomy,
cingulotomy and limbic leukotomy – all aim to interrupt the connection between
the cortex and the basal ganglia and related structures. Current stereotactic
surgical techniques involve the creation of precise lesions, which are often only
10 to 20 mm, to specific tracts. These procedures have often been done with
radiofrequency heated electrodes andmore recently, with gamma knife techniques.
Postsurgical risks have been minimized, and in some cases cognitive function
and personality traits improve along with symptoms of OCD.
Data compiled from a number of small studies have yielded success rates
of 25 to 84% with treatment. However, most samples are small, and the
procedures have often differed in both lesion location and size, making it difficult
to compare them. However, in a recent prospective long-term follow-up study,
all 44 patients received the same procedure (cingulotomy), although some had
single procedures and others multiple procedures (Dougherty et al., 2002). This study had several
important findings. Clinical improvement occurred in 32 to 45% of
patients, depending on the criteria used to rate full or partial response, and
the average effect size was 1.27, comparable to that seen in pharmacologic
trials (1.09–1.53). However, these changes were not immediately apparent
postoperatively, and most patients were encouraged to engage in pharmacotherapy
and/or behavior therapy postopera-tively. The longitudinal follow-up component
of the study, which was a mean duration of 32 months, allowed the researchers
to assess the longer-term impact of the procedure in ways other studies could
not. Of particular note, patients continued to show improvement for up to 29
months after surgery without receiving further procedures. As a result, the authors
noted that the typical 6-month wait before deciding whether to repeat and
extend the lesion may be too brief. In conclusion, neurosurgical treatments
offer hope to some of the most severely ill and treatment-resist-ant patients
and should therefore be considered. However, which surgical lesions are most
effective in which patients still needs much more study.
Related Topics